Case of the Week #643
(1) Monash Ultrasound for Women; (2) Centro Médico Recoletas, Valladolid, Spain
38-year-old woman with no significant previous medical history presented for her first scan at 13 weeks. This was her first pregnancy and was conceived through in vitro fertilization abroad.
View the Answer Hide the Answer
Answer
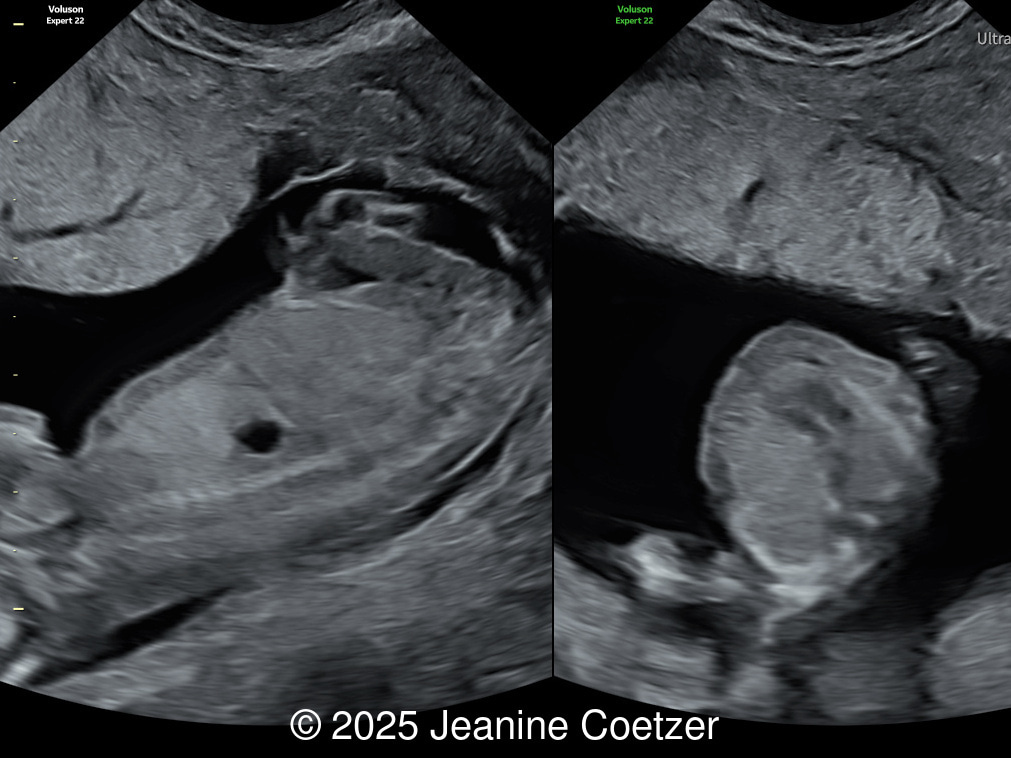
We present a case of Congenital Diaphragmatic Hernia diagnosed in the first trimester.
Our imaging revealed a left-sided congenital diaphragmatic hernia with the stomach located in the left hemithorax causing significant mediastinal shift, and right cardiac axis deviation. The four cardiac chambers and outflow tracts appeared normal. Invasive genetic testing was declined. The parents were committed to the pregnancy and did not return for follow up.
Discussion
Congenital diaphragmatic hernia is a severe malformation characterized by a defect in the diaphragm through which the abdominal viscera migrate into the fetal thorax [1,2]. The most widely used classification system is based on anatomical location [2,3]. Approximately 90% of all congenital diaphragmatic hernias are classified as being posterolateral (Bochdalek type), with 85% occurring on the left side, 13% on the right, and 2% are bilateral. Defects in the most anterior portion of the diaphragm are rare. Morgagni hernias make up 9% of total and are usually accompanied by a hernia sac. Other anterior hernias accompany Cantrell's pentalogy, and central hernias primarily involve the central tendinous portion of the diaphragm.
According to a meta-analysis including nearly 8 million live and stillbirths, the average prevalence of congenital diaphragmatic hernia is 1 in 4080 births [4]. Most cases (60%) are isolated, without other anatomic or chromosomal defects, however 40% are complex and present with associated anomalies [5]. More than 50 different genetic causes are associated with congenital diaphragmatic hernia [6], including aneuploidies (trisomies 13, 18 and 21), chromosome copy number variants (tetrasomy 12p, Pallister-Killian syndrome), single gene mutations (Simpson-Golabi-Behmel, Cornelia de Lange, Donnai-Barrow syndrome), and syndromes with unknown genetic etiologies (Fryns syndrome). It has been postulated that the embryogenesis of congenital diaphragmatic hernia is due to a failure of fusion of the pleuroperitoneal folds with the septum transversum, the esophageal mesentery, and lateral body walls during the 8th week of gestation. Abdominal organs migrate into the thorax, compressing the ipsilateral lung, leading to pulmonary hypoplasia and abnormal development of pulmonary vascularization. However, there is growing evidence that ipsilateral lung abnormalities are not simply caused by intrathoracic herniation of the abdominal organs. The dual‑hit hypothesis proposes that impairment of both lungs occurs before the failed diaphragmatic closure and mechanical compression [7].
Most congenital diaphragmatic hernias are first suspected at screening ultrasounds between the 18th to 22nd weeks of gestation, however they have been identified as early as the first trimester of pregnancy. Approximately 50% of congenital diaphragmatic hernias are identified on the first trimester ultrasound [8]. Paladini and Volpe [9] consider diaphragmatic hernia an “evolving” lesion; Although the defect occurs in early stages of gestation, the moment at which the viscera herniate is extremely variable and ranges from the late first trimester to the first hours of life. For this reason, some cases are not detectable in the first trimester [10]. Fetal morphological assessment is usually performed in the context of combined screening for chromosomal abnormalities. Nuchal translucency is increased in almost 40% of fetuses with congenital diaphragmatic hernia [8] and may be the consequence of venous congestion in the head and neck due to mediastinal compression and poor venous return [11]. The diagnosis of diaphragmatic hernia in the first trimester has been identified in fetuses with normal [12,13] and increased [10,11,14-19] nuchal translucency. In most cases, the diagnosis of congenital diaphragmatic hernia is indirect after detecting the displacement of the heart and mediastinum caused by the abnormal intrathoracic position of the stomach and/or other viscera migrated from the abdomen; however, these signs may not be so evident in the first trimester [12,13,16,18-20]. Sagittal and parasagittal views can visualize the absence of the hypoechoic contour of the diaphragm, a tortuous path of the inferior vena cava and a cephalad course of the superior mesenteric artery [9,21]. Abuhamad and Chaoui [20] consider that the key findings for the diagnosis of diaphragmatic hernia in the first trimester are a more cranial position of the stomach in the coronal view of the thorax and abdomen, the slight change of cardiac position in the four-chamber view, and the abnormal course of the ductus venosus in the abdomen.
The most important prognostic factor for fetuses with congenital diaphragmatic hernia is the association with chromosomal abnormalities or genetic syndromes. An invasive test (usually amniocentesis) is mandatory for genetic testing, which should include karyotyping, CGH array, and, if possible, whole-exome sequencing. For isolated cases, the most accepted prognostic parameters in the second and third trimesters are the assessment of the amount of the lung tissue (evaluated by the observed/expected lung-to-head ratio -o/e LHR-) and the presence of liver herniation. This can be difficult to assess in the first trimester. Therefore, the association of congenital diaphragmatic hernia with increased nuchal translucency and even the fact of early diagnosis itself could be more predictive of outcome in the first trimester. The association of increased nuchal translucency and congenital diaphragmatic hernia suggests a poor outcome, even after ruling out chromosomal or genetic defects [17]. The neonatal mortality rate decreases significantly with increasing gestational age at diagnosis, with rates of approximately 60%, 40%, and 10% in the first, second, and third trimesters, respectively, with similar results for respiratory morbidity (persistent pulmonary hypertension) [22].
The differential diagnosis of congenital diaphragmatic hernia includes any intrathoracic lesion that displaces the fetal heart or lungs, including cystic (congenital pulmonary airway malformation, bronchogenic cyst) and solid lesions (bronchopulmonary sequestration, bronchial atresia, and mediastinal teratoma) [1,23,24]. In these cases, the intra-abdominal organs do not shift into the thorax, and characteristic findings can be found: multiple cystic lesions in congenital malformations of the pulmonary airways and a systemic feeding vessel in bronchopulmonary sequestration.
The recurrence risk for apparently isolated congenital diaphragmatic hernia is approximately 1-2%. While this recurrence risk is low, the recurrence risk increases 20-fold compared to the incidence of this pathology in the general population. Therefore, subsequent pregnancies should be monitored with fetal imaging [5].
References
- Russo FM, van der Merwe J, Aertsen M, Devlieger R, Lewi L, De Catte L, and Deprest J. Congenital Diaphragmatic Hernia. In: Copel JA, ed. Obstetric Imaging. Fetal diagnosis and care, 3rd ed. Elsevier, Philadelphia, PA, 2026; pag 320- 326.e1.
- Chandrasekharan PK, Rawat M, Madappa R, et al. Congenital Diaphragmatic hernia - a review. Matern Health Neonatol Perinatol. 2017 Mar 11;3:6.
- Pober BR. Overview of epidemiology, genetics, birth defects, and chromosome abnormalities associated with CDH. Am J Med Genet C Semin Med Genet. 2007 May 15;145C(2):158-171.
- Skari H, Bjornland K, Haugen G, et al. Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg. 2000 Aug;35(8):1187-1197.
- Pober BR. Genetic aspects of human congenital diaphragmatic hernia. Clin Genet. 2008 Jul;74(1):1-15.
- Wynn J, Yu L, Chung WK. Genetic causes of congenital diaphragmatic hernia. Semin Fetal Neonatal Med. 2014 Dec;19(6):324-330.
- Keijzer R, Liu J, Deimling J, et al. Dual-hit hypothesis explains pulmonary hypoplasia in the nitrofen model of congenital diaphragmatic hernia. Am J Pathol. 2000 Apr;156(4):1299-1306.
- Syngelaki A, Chelemen T, Dagklis T, et al. Challenges in the diagnosis of fetal non-chromosomal abnormalities at 11-13 weeks. Prenat Diagn. 2011 Jan;31(1):90-102.
- Paladini D and Volpe P. Thoracic Anomalies. In: Ultrasound of congenital fetal anomalies: differential diagnosis and prognostic indicators, 3rd ed. CRC Press, Boca Raton, FL, 2024; pag 419-457.
- Sepulveda W, Wong AE, Casasbuenas A, et al. Congenital diaphragmatic hernia in a first-trimester ultrasound aneuploidy screening program. Prenat Diagn. 2008 Jun;28(6):531-534.
- Sebire NJ, Snijders RJ, Davenport M, et al. Fetal nuchal translucency thickness at 10-14 weeks' gestation and congenital diaphragmatic hernia. Obstet Gynecol. 1997 Dec;90(6):943-946.
- Daskalakis G, Anastasakis E, Souka A, et al. First trimester ultrasound diagnosis of congenital diaphragmatic hernia. J Obstet Gynaecol Res. 2007 Dec;33(6):870-872.
- Sousa Ferreira B, Martins M, Correia A, Moutinho O. Congenital diaphragmatic hernia: a rare first trimester prenatal diagnosis. BMJ Case Rep. 2025 Feb 24;18(2):e263713.
- Lam YH, Tang MH, Yuen ST. Ultrasound diagnosis of fetal diaphragmatic hernia and complex congenital heart disease at 12 weeks' gestation--a case report. Prenat Diagn. 1998 Nov;18(11):1159-1162.
- Lam YH, Eik-Nes SH, Tang MH, et al. Prenatal sonographic features of spondylocostal dysostosis and diaphragmatic hernia in the first trimester. Ultrasound Obstet Gynecol. 1999 Mar;13(3):213-215.
- Varlet F, Bousquet F, Clemenson A, et al. Congenital diaphragmatic hernia. Two cases with early prenatal diagnosis and increased nuchal translucency. Fetal Diagn Ther. 2003 Jan-Feb;18(1):33-35.
- Spaggiari E, Stirnemann J, Ville Y. Outcome in fetuses with isolated congenital diaphragmatic hernia with increased nuchal translucency thickness in first trimester. Prenat Diagn. 2012 Mar;32(3):268-271.
- Jensen KK, Sohaey R. First-Trimester Diagnosis of Congenital Diaphragmatic Hernia. Ultrasound Q. 2016 Dec;32(4):370-372.
- Di Gregorio DM, Martin D, Mansilla L. First Trimester Cystic Hygroma: Herald to Early Diagnosis of Congenital Diaphragmatic Hernia. P R Health Sci J. 2021 Mar;40(1):53-55.
- Abuhamad A, Chaoui R. The Fetal Chest. In: First trimester ultrasound diagnosis of fetal abnormalities, 1st ed. Wolters Kluwer Heath, Philadelphia, PE, 2018; pag 179-190.
- Lakshmy RS, Agnees J, Rose N. The Upturned Superior Mesenteric Artery Sign for First-Trimester Detection of Congenital Diaphragmatic Hernia and Omphalocele. J Ultrasound Med. 2017 Mar;36(3):583-592.
- Bouchghoul H, Senat MV, Storme L, et al; Center for Rare Diseases for Congenital Diaphragmatic Hernia. Congenital diaphragmatic hernia: does gestational age at diagnosis matter when evaluating morbidity and mortality? Am J Obstet Gynecol. 2015 Oct;213(4):535.e1-7.
- Claus F, Sandaite I, DeKoninck P, et al. Prenatal anatomical imaging in fetuses with congenital diaphragmatic hernia. Fetal Diagn Ther. 2011;29(1):88-100.
- Kosiński P, Wielgoś M. Congenital diaphragmatic hernia: pathogenesis, prenatal diagnosis and management - literature review. Ginekol Pol. 2017;88(1):24-30.
Discussion Board
We appreciate your patience as we review all submitted answers. Check back soon to see if you were correct!