Case of the Week #637
(1) Vinmec Healthcare System, Hanoi, Vietnam; (2) University of Texas, Southwestern Medical Center, Plano, Texas, USA; (3) UCSF Health, San Francisco, California, USA
A woman underwent routine prenatal screening at 13 weeks. The non-invasive prenatal test (NIPT) showed low risk for common aneuploidies including trisomy 21, 18, and 13. However, first-trimester anomaly scan revealed multiple fetal anomalies.
Please describe the abnormalities and provide a syndromic diagnosis that best fits the presentation.







View the Answer Hide the Answer
Answer
We present a case of Triploidy with a 69,XXY chromosomal complement and open spina bifida in the first trimester.
Our imaging revealed the following significant fetal abnormalities:
- Thin nasal bone
- Open spina bifida in the sacral region with dry brain sign, crash sign, BS/BSOB >1, and a lesion at the sacral coccygeal spine. The spinal lesion observed in the sacral region is characterized by a posterior vertebral arch defect and a protruding meningeal sac.
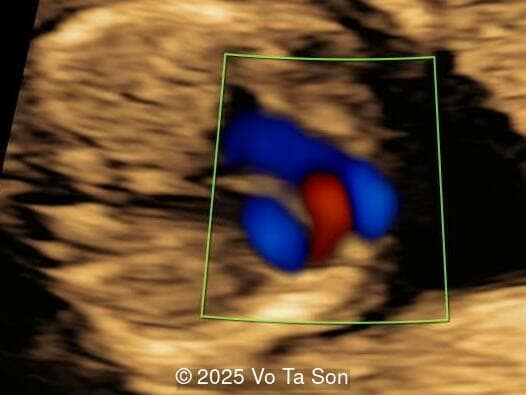
- Ventricular septal defect (VSD)
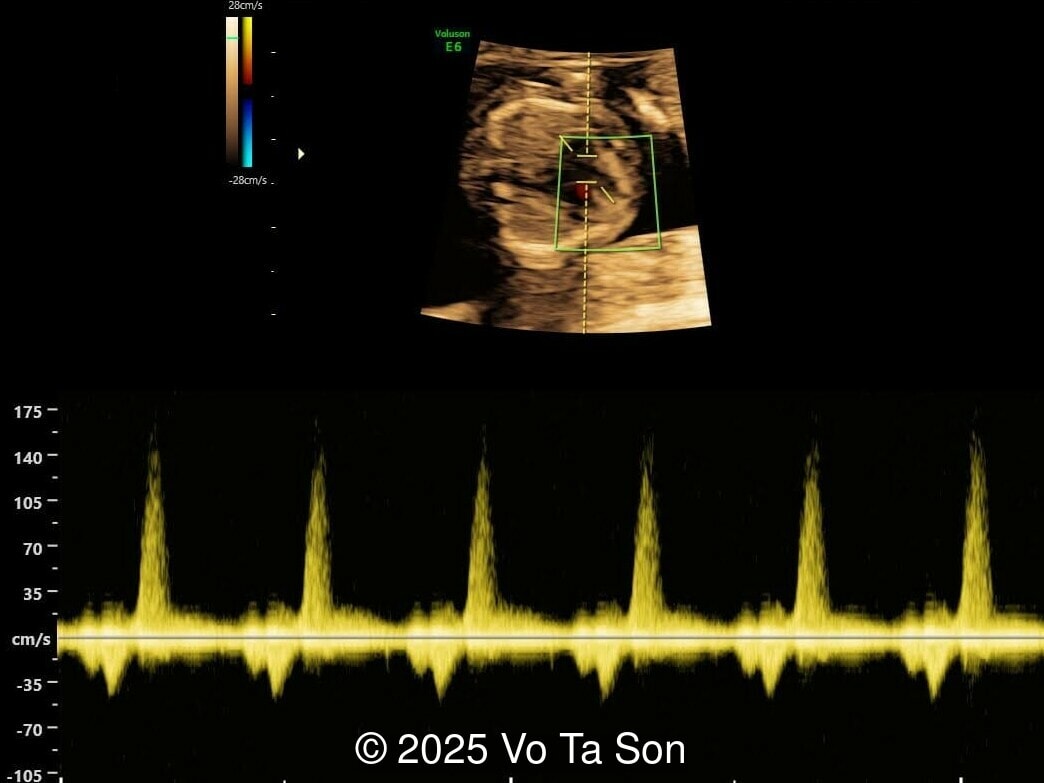
- Tricuspid valve regurgitation
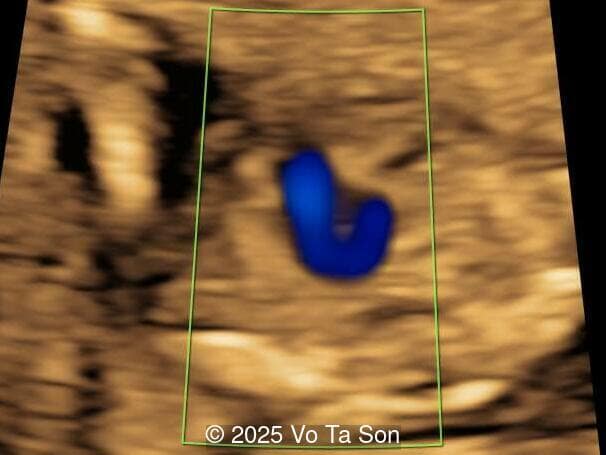
- Right aortic arch
- Cystic-appearing placenta, suggestive of partial molar changes
Given the discordance between the low-risk NIPT result and the concerning ultrasound findings, chorionic villus sampling was performed. Karyotype results revealed triploidy with a 69,XXY chromosomal complement, consistent with diandric triploidy (paternal origin). This finding correlated well with the ultrasound abnormalities, particularly the cystic placenta and multiple fetal structural defects.
Discussion
Triploidy, a lethal chromosomal disorder characterized by the presence of three complete sets of chromosomes (69,XXX, 69,XXY, or 69,XYY), typically leads to early pregnancy loss or perinatal mortality and can result in maternal complications such as pre-eclampsia and persistent trophoblastic disease [1]. The 69,XXX and 69,XXY chromosome compliment is more commonly identified than 69,XYY [2,3]. The estimated incidence of triploidy at 11 to 14 weeks gestation is approximately 1 in 3270 to 6,600 pregnancies [1,4]. Due to the high rate of spontaneous pregnancy loss in the first trimester, diagnosis in the second trimester is rare, decreasing to an incidence of approximately 1 in 27,000 [5]. The additional haploid set of chromosomes can be of paternal origin, called diandric triploidy, or maternal origin, known as digynic triploidy. In diandric triploidy, the extra set of chromosomes results from either two sperm fertilizing a single ovum, or a diploid sperm, which occurs from complete nondisjunction during spermatogenesis, fertilizing a single ovum. When the extra set of chromosomes is of maternal origin, a sperm fertilizes a diploid ovum, which occurs due to nondisjunction during meiosis, fertilization of a primary oocyte, or retention of a polar body [6,7]. There is no consensus on whether digyny or diandry is the more common cause of human triploidy [2,3,8].
Prenatal detection of triploidy often hinges on identifying a combination of ultrasonographic anomalies, particularly intrauterine growth restriction, structural malformations, and characteristic placental or maternal serum findings. A detection rate of approximately 83% has been observed at the first trimester screening [1]. Digynic and diandric triploidy have specific features which can be differentiated with ultrasound. Nuchal translucency can be thickened in both types of triploidy, but is often within the normal range [6,7]. Mcfadden et al was the first to describe the phenotype of triploidy [9,10]. Diandric triploidy (type 1) is typically associated with a normally grown fetus and a large, hyperplastic placenta with partial hydatidiform mole changes. Conversely in digynic triploidy (type 2), a small placenta is seen in the setting of severe growth restriction. The fetus in digynic triploidy often has a short crown-rump length and a significant difference between the head and abdominal circumference, usually of more than two weeks gestational age. The size discrepancy between the head and abdominal circumference is a pathognomonic sign of digynic triploidy [6,7].
If a triploid fetus survives to the second trimester, structural anomalies can be detected by ultrasound and occur in approximately 44-49% of fetuses [4,11]. These include anomalies of the extremities (syndactyly of the third and fourth fingers, clubfeet), central nervous system (holoprosencephaly, Dandy-Walker malformation, agenesis of the corpus callosum, neural tube defects), face (micrognathia, microphthalmia), as well as omphalocele, cardiac anomalies, and renal anomalies [6,7]. The most common findings are syndacyly, occurring in approximately 70% of cases [11], and central nervous system anomalies, which are found in approximately 40% of cases [11], with myelomeningocele found in 9-13% of fetuses with triploidy [8,11-12]. Cardiac defects occur in 13%, of which 9% are ventricular septal defect [11]. If these defects are seen in a growth-restricted fetus, triploidy should be considered in the differential diagnosis and amniocentesis offered, especially if the placenta is enlarged and contains cysts. Features of a partial hydatidiform mole occurs in 24-33% of cases with triploidy [4,11]. Additionally, theca lutein cysts may develop in the maternal ovaries due to high levels of human chorionic gonadotropin [6,7].
In a study reviewing first trimester risk assessment, which included nuchal translucency, maternal age, and maternal serum markers (β-hCG, PAPP-A), 18% (5/28) of patients with triploidy screened negative, however, 2 of the cases were found to have anomalies on the first trimester screening ultrasound and the other 3 cases had anomalies noted on the second trimester ultrasound [1]. Thus approximately 11% of confirmed triploidy cases screened negative on serum testing and had no anomalies detected on first trimester ultrasound [1]. This is consistent with a study by Huang et al who reviewed maternal serum tests performed in the second trimester and found a screen-negative result for 10% of pregnancies with triploidy [5]. Other noninvasive techniques have been studied to make the diagnosis of triploidy such as cell‐free DNA (cfDNA) based NIPT. Single nucleotide polymorphism (SNP)‐based NIPT can identify triploidy by detecting the presence of the additional haploid chromosome set, however, the SNP pattern seen with triploidy can sometimes be difficult to distinguish from the pattern seen with dizygotic twins, and in approximately 60% of cases, positive results can be attributed to vanished twins. When an extra haplotype is detected on SNP‐based NIPT, only 11% was due to triploidy [13].
In conclusion, first trimester non-invasive testing and ultrasound identifies up to 90% of pregnancies affected by triploidy. If on second trimester ultrasound, a fetus is noted to be growth restricted with relative macrocephaly or have a large, cystic placenta, in addition to structural anomalies, such as syndactyly and central nervous system anomalies, genetic counseling and invasive confirmatory testing, typically via amniocentesis or chorionic villous sampling, are vital to confirm the diagnosis.
References
[1] Engelbrechtsen L, Brøndum-Nielsen K, Ekelund C, et al. Detection of triploidy at 11-14 weeks' gestation: a cohort study of 198 000 pregnant women. Ultrasound Obstet Gynecol. 2013 Nov;42(5):530-5.
[2] McFadden DE, Langlois S. Parental and meiotic origin of triploidy in the embryonic and fetal periods. Clin Genet. 2000 Sep;58(3):192-200.
[3] Zaragoza MV, Surti U, Redline RW, et al. Parental origin and phenotype of triploidy in spontaneous abortions: predominance of diandry and association with the partial hydatidiform mole. Am J Hum Genet. 2000 Jun;66(6):1807-20.
[4] Jauniaux E, Brown R, Snijders RJ, et al. Early prenatal diagnosis of triploidy. Am J Obstet Gynecol. 1997 Mar;176(3):550-4.
[5] Huang T, Alberman E, Wald N, et al. Triploidy identified through second-trimester serum screening. Prenat Diagn. 2005 Mar;25(3):229-33.
[6] Abuhamad, A, et al. "First Trimester Screening for Chromosomal Aneuploidies". First Trimester Ultrasound Diagnosis of Fetal Abnormalities. Philadelphia: Wolters Kluwer Health, 2018. pgs 87-91.
[7] Doubilet, P, et al. "Chromosomal Anomalies". Atlas of Ultrasound in Obstetrics and Gynecology: A Multimedia Reference (3rd Edition). Philadelphia: Wolters Kluwer, 2019. pgs 294-298.
[8] Baumer A, Balmer D, Binkert F, et al. Parental origin and mechanisms of formation of triploidy: a study of 25 cases. Eur J Hum Genet. 2000 Dec;8(12):911-7.
[9] McFadden DE, Kalousek DK. Two different phenotypes of fetuses with chromosomal triploidy: correlation with parental origin of the extra haploid set. Am J Med Genet. 1991 Mar 15;38(4):535-8.
[10] McFadden DE, Kwong LC, Yam IY, et al. Parental origin of triploidy in human fetuses: evidence for genomic imprinting. Hum Genet. 1993 Nov;92(5):465-9.
[11] Toufaily MH, Roberts DJ, Westgate MN, et al. Triploidy: Variation of Phenotype. Am J Clin Pathol. 2016 Jan;145(1):86-95.
[12] Ferreira AFA, Syngelaki A, Smolin A, et al. Posterior brain in fetuses with trisomy 18, trisomy 13 and triploidy at 11 to 13 weeks’ gestation. Prenat Diagn. 2012 Sep;32(9):854-8.
[13] Kantor V, Jelsema R, Xu W, et al. Non-invasive prenatal screening for fetal triploidy using single nucleotide polymorphism-based testing: Differential diagnosis and clinical management in cases showing an extra haplotype. Prenat Diagn. 2022 Jul;42(8):994-999.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Padman KG United Kingdom Sonographer

Mayank Chowdhury India Physician
Boujemaa Oueslati Tunisia Physician

Peter conner Sweden Physician

Victoria Giang Viet Nam Physician

Elena Andreeva Russian Federation Physician

Muradiye YILDIRIM Turkey Physician

Ionut Valcea Romania Physician

Hien Nguyen Van Viet Nam Physician

Kareem Haloub Australia Physician

Annette Reuss Germany Physician

Arati Appinabhavi India Physician

Ricardo Burgos El Salvador Physician

Le Tien Dung Viet Nam Physician

Le Duc Viet Nam Physician
Marius Bogdan Muresan Romania Physician

jimena salcedo Spain Physician
Maria Bulanova Russian Federation Physician