Case of the Week #634
(1) Polish Mother's Research Institute, Department of Genetics; (2) Department of Pediatrics, Division Pediatric Propedeutics and Rare Disorders, Wroclaw Medical University, Poland; (3) Centro Médico Recoletas, Valladolid, Spain
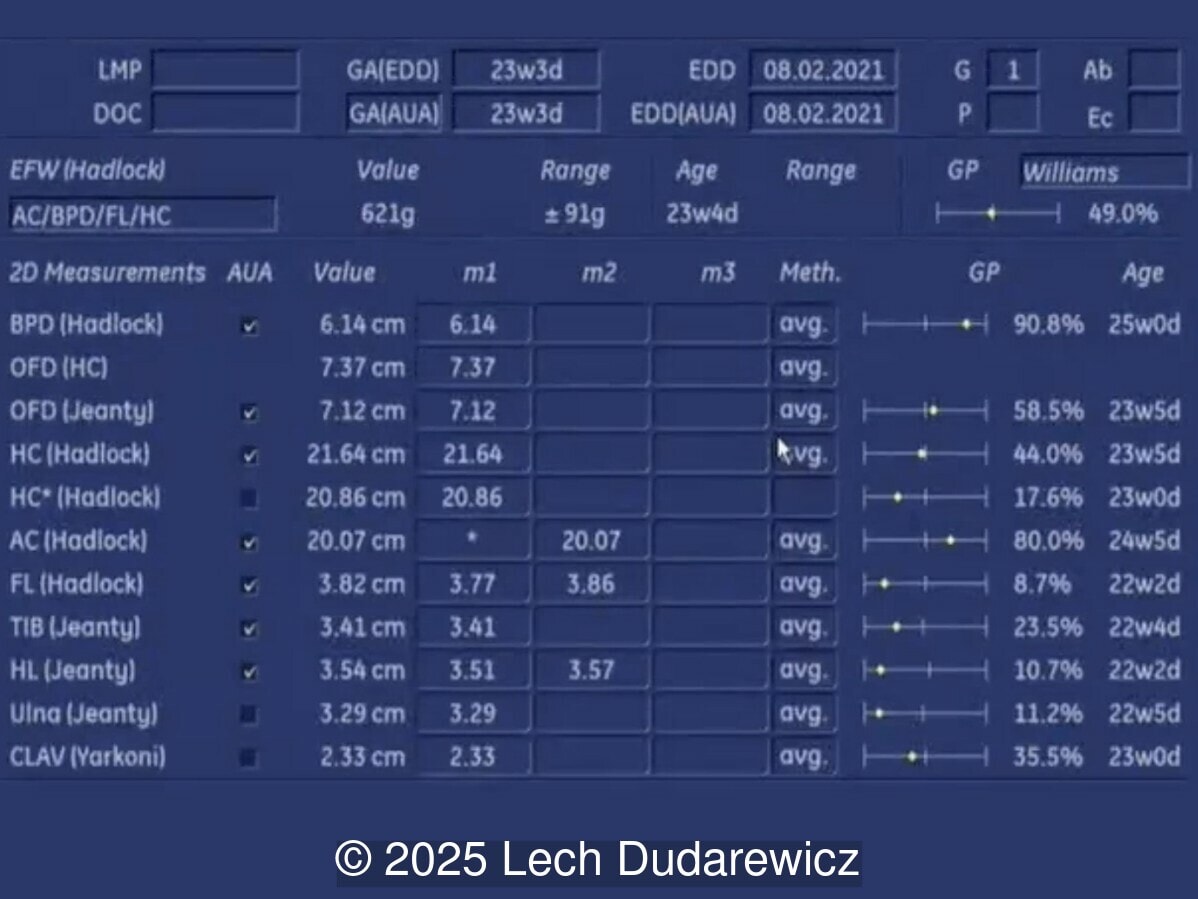
A 30-year-old primigravid woman was referred to our office at 23 weeks, 3 days of gestation due to suspected fetal dysmorphic features and a single umbilical artery observed on routine mid-trimester ultrasound. Ultrasound findings are shown below. The patient had polyhydramnios. The remainder of the scan was normal.
What is the most likely diagnosis?
View the Answer Hide the Answer
Answer
We present a case of Aarskog-Scott Syndrome.
Prenatal ultrasound demonstrated the following findings:
- Flattened facial profile due to maxillary hypoplasia and a short nose with a broad nasal bridge
- Hypertelorism
- Mild brachydactyly of both hands
- Broad feet and hands
- Brachycephaly
- Single umbilical artery
- Mild polyhydramnios (AFI = 22.9 cm, MVP = 7.2 cm)
- Short humerus
Cardiac anatomy and neurosonography appeared normal. Genetic testing, including amniocentesis with chromosomal microarray and whole exome sequencing, was recommended, but declined by the patient. Postnatal whole exome sequencing was performed and revealed a pathogenic mutation in FGD1, confirming the diagnosis.
Discussion
Aarskog-Scott syndrome (OMIM #305400), also known as facio-digito-genital syndrome, is a rare developmental disorder primarily affecting males and characterized by distinct craniofacial, skeletal, and genital abnormalities [1]. In 1970, Dagfinn Aarskog, a Norwegian pediatrician and geneticist, described seven males in three generations of a family with a syndrome of short stature, round facies, hypertelorism, short nose with anteverted nostrils, broad upper lip with marked philtrum, inguinal hernia, undescended testes, and a scrotal skin fold extending ventrally around the base of the penis. All the affected subjects had normal motor and mental development [2]. A year later, Charles Scott, Jr, an American geneticist, reported three brothers with similar characteristics and some additional findings (small hands with short fingers and joint hypermobility) which completed the definition of the entity [3].
The exact incidence of this pathology is unknown due to its wide clinical variability and mild physical signs. The population prevalence is estimated to be approximately 1 in 25,000 [4]. Although sex-influenced autosomal dominant and recessive inheritance patterns have been described [5,6], only an X-linked recessive form associated with mutations in the FGD1 gene is recognized as the cause of this syndrome [7,8]. To date, 147 variants have been published (https://databases.lovd.nl/shared/genes/FGD1) including missense, nonsense, deletions, insertions and gross rearrangements [4]. The FGD1 gene (formerly named FDG1, changed to conform with standardized genetic nomenclature in early 2000's), located on the Xp11.22 region of the X chromosome, encodes a guanine nucleotide exchange factor (GEF) that activates Cdc42, which participates directly in cytoskeletal organization, growth regulation, and normal embryonic development in all mammals [9]. The clinical phenotype does not seem to correlate with the type and position of the mutation [10].
Aarskog-Scott syndrome is recognized as a pleiotropic disorder (multiple and distinct phenotypic traits caused by a single gene) involving the skeletal system, face, and external genitalia, with highly variable expressivity even within the same family [11,12]. The most characteristic findings are proportionate short stature, short limbs (usually rhizomelic), broad hands and feet, genital anomalies (shawl scrotum), and facial dysmorphism. The name facio-digito-genital dysplasia is justified in view of the high prevalence rates of hypertelorism (94.8%), brachydactyly (62.1%), and shawl scrotum (79.3%) [10]. Organizing clinical findings according to their prevalence is useful for management of patients with rare genetic diseases, facilitating the selection of genetic tests that provide a definitive diagnosis. Teebi et al [13] reviewed more than 130 males with Aarskog-Scott syndrome published up to 1993 and divided their findings into primary and secondary diagnostic criteria according to their frequency. Primary manifestations, which are present in more than 80% of reported patients, include short stature, hypertelorism, short nose with anteverted nares, maxillary hypoplasia, a crease below the lower lip, mild interdigital webbing with short and broad hands, short fifth finger with clinodactyly, and shawl scrotum. Secondary criteria are less frequent, present in 50 to 70% of the patients, and include abnormal auricles with fleshy lobules, posteriorly angulated ears, widow’s peak, ptosis, downward slant of palpebral fissures, joint hyperextensibility, broad feet with bulbous toes, cryptorchidism, inguinal hernia, and prominent umbilicus. More recently, Zanetti et al. classified the findings into primary (prevalence ≥ 50%), secondary (between 30% and 49%), and additional (between 15% and 29%) criteria [10]. Mental retardation and/or attention deficit/hyperactivity disorder may be part of the Aarskog-Scott syndrome phenotype [14,15]. Patients with mental impairment are only mildly affected, with learning and behavioral disabilities often confined to early childhood [16]. Facial features and the typical morphology of the hands change with age (hypertelorism less evident, forehead less prominent, and face more elongated), making clinical diagnosis difficult in adults.
Affected males inherit the pathogenic variant from their carrier mothers. Each son of a carrier woman has a 50% chance of being affected and each daughter has a 50% chance of being a carrier. Female carriers may present a milder phenotype than males, possibly due to the X-chromosome inactivation pattern, showing minor dysmorphic features such as short stature, hypertelorism, round face and characteristic hands and feet, with abnormal migration of the labioscrotal folds having been described in a girl from a family with Aarskog-Scott syndrome [11,17].
Prenatal diagnosis of Aarskog-Scott syndrome is rare. To the best of our knowledge, only four cases are documented in the literature, identified in high-risk pregnancies [12,18,19]. Although it is often diagnosed only postnatally based on characteristic physical features and developmental history, certain distinct but subtle ultrasound signs may raise prenatal suspicion, especially in the second or early third trimester. In our case, retrospective review of the prenatal ultrasound images and video clips, following genetic confirmation, allowed us to better appreciate subtle and previously overlooked features consistent with the phenotype commonly described in Aarskog-Scott syndrome:
1. Craniofacial Anomalies:
- Hypertelorism – a consistent and sometimes striking feature. It may be detectable by measuring interorbital distance or binocular diameter.
- Short and broad nasal bridge, small and short nose with anteverted nostrils and short maxillae, leading to flattened midface also called midfacial hypoplasia ("Binder-like" profile).
- Large earlobes, often low-set
- Mild brachycephaly – occasionally present and observable as a shortened occipitofrontal diameter with a relatively preserved biparietal diameter.
2. Skeletal Findings:
- Mild shortening of long bones, especially the humerus and femur, though still within the borderline normal range. These features may mimic constitutional growth delay but should be considered suspicious in the proper context.
- Broad hands with brachydactyly, often subtle and difficult to appreciate
- Broad feet or broad first toes – best seen in plantar views.
3. Genital Features:
- Shawl scrotum, manifestation of a penoscrotal transposition with the skin of the scrotum surrounding the phallus frontally, is a highly suggestive finding, although not assessable prenatally.
- Cryptorchidism – undescended testes may be suspected with careful examination of the scrotal sac, although only in the late third trimester, confirmation often awaits postnatal physical examination.
While none of these features are pathognomonic on their own, their combination can be specific for Aarskog-Scott syndrome and should prompt further genetic evaluation. Intrauterine growth retardation and shortening of the long bones are among the most typical prenatal findings of this condition, but this feature is particularly nonspecific [1,20]. Umbilical anomalies, including single umbilical artery, flat configuration of the umbilicus, and protruding umbilicus are not considered specific, but have been reported in association with Aarskog-Scott syndrome. [12, 21]
Congenital malformations have been described in patients with Aarskog-Scott syndrome, such as congenital heart defects (septal defects, aortic root dilatation), thickened corpus callosum, gyration abnormalities, cerebrovascular dysplasia, inguinal hernia, cleft lip and palate, cervical spine abnormalities (spina bifida occulta, fused cervical vertebrae), dolichomegasigmoid, and anal anomalies [1,19,22-25]. Additional clinical studies are needed to determine whether these malformations are a coincidence or rare manifestations of Aarskog syndrome.
In the presence of findings suggestive of Aarskog-Scott syndrome, the recommended genetic diagnostic flow includes targeted single-gene sequencing of the FGD1 gene, multi-gene panels for syndromic short stature or facial dysmorphism, chromosomal microarray (CMA), and whole exome sequencing (WES) in cases with negative CMA. Carrier testing in mothers of affected male fetuses is crucial to confirm inheritance pattern and assess recurrence risk.
The differential diagnosis includes Noonan syndrome, Robinow syndrome, and SHORT (Short stature, Hyperextensibility of joints, Ocular depression, Rieger anomaly and Teething delay) syndrome [4,10,18]. Noonan syndrome shows significant clinical overlap with short stature, hypertelorism, genital anomalies, and ptosis. Robinow syndrome also has many clinical similarities (short stature, hypertelorism, facial features), but these individuals never present a shawl scrotum.
References
[1] Jeanne M, Ronce N, Remizé S, et al. Aarskog-Scott syndrome: a clinical study based on a large series of 111 male patients with a pathogenic variant in FGD1 and management recommendations. J Med Genet. 2025 Mar 20;62(4):258-267.
[2] Aarskog D. A familial syndrome of short stature associated with facial dysplasia and genital anomalies. Birth Defects Orig Artic Ser. 1971 May;7(6):235-239.
[3] Scott CI. Unusual facies, joint hypermobility, genital anomaly and short stature: a new dysmorphic syndrome. Birth Defects Orig Artic Ser. 1971 May;7(6):240-246.
[4] Orrico A, Galli L, Clayton-Smith J, Fryns JP. Clinical utility gene card for: Aarskog-Scott Syndrome (faciogenital dysplasia) - update 2015. Eur J Hum Genet. 2015 Apr;23(4).
[5] Grier RE, Farrington FH, Kendig R, Mamunes P. Autosomal dominant inheritance of the Aarskog syndrome. Am J Med Genet. 1983 May;15(1):39-46.
[6] Teebi AS, Naguib KK, Al-Awadi S, Al-Saleh QA. New autosomal recessive faciodigitogenital syndrome. J Med Genet. 1988 Jun;25(6):400-406.
[7] Berman P, Desjardins C, Fraser FC. The inheritance of the Aarskog facial-digital-genital syndrome. J Pediatr. 1975 Jun;86(6):885-891.
[8] Pasteris NG, Cadle A, Logie LJ, et al. Isolation and characterization of the faciogenital dysplasia (Aarskog-Scott syndrome) gene: a putative Rho/Rac guanine nucleotide exchange factor. Cell. 1994 Nov 18;79(4):669-678.
[9] Gorski JL, Estrada L, Hu C, Liu Z. Skeletal-specific expression of Fgd1 during bone formation and skeletal defects in faciogenital dysplasia (FGDY; Aarskog syndrome). Dev Dyn. 2000 Aug;218(4):573-586.
[10] Zanetti Drumond V, Sousa Salgado L, Sousa Salgado C, et al. The Prevalence of Clinical Features in Patients with Aarskog-Scott Syndrome and Assessment of Genotype-Phenotype Correlation: A Systematic Review. Genet Res (Camb). 2021 Feb 2;2021:6652957.
[11] Orrico A, Galli L, Cavaliere ML, et al. Phenotypic and molecular characterisation of the Aarskog-Scott syndrome: a survey of the clinical variability in light of FGD1 mutation analysis in 46 patients. Eur J Hum Genet. 2004 Jan;12(1):16-23.
[12] Shalev SA, Chervinski E, Weiner E, et al. Clinical variation of Aarskog syndrome in a large family with 2189delA in the FGD1 gene. Am J Med Genet A. 2006 Jan 15;140(2):162-165.
[13] Teebi AS, Rucquoi JK, Meyn MS. Aarskog syndrome: report of a family with review and discussion of nosology. Am J Med Genet. 1993 Jun 15;46(5):501-509.
[14] Logie LJ, Porteous ME. Intelligence and development in Aarskog syndrome. Arch Dis Child. 1998 Oct;79(4):359-360.
[15] Orrico A, Galli L, Buoni S, et al. Attention-deficit/hyperactivity disorder (ADHD) and variable clinical expression of Aarskog-Scott syndrome due to a novel FGD1 gene mutation (R408Q). Am J Med Genet A. 2005 May 15;135(1):99-102.
[16] Fryns JP. Aarskog syndrome: the changing phenotype with age. Am J Med Genet. 1992 Apr 15-May 1;43(1-2):420-427.
[17] Moraes SG, Guerra-Junior G, Maciel-Guerra AT. Female counterpart of shawl scrotum in Aarskog-Scott syndrome. Int Braz J Urol. 2006 Jul-Aug;32(4):459-461.
[18] Sepulveda W, Dezerega V, Horvath E, Aracena M. Prenatal sonographic diagnosis of Aarskog syndrome. J Ultrasound Med. 1999 Oct;18(10):707-710.
[19] Hubaishi N, Cherifi F, Taka MK, et al. Aarskog–Scott syndrome – prenatal ultrasound diagnosis in a case with positive family history. Hamdan Medical Journal. Jul–Sep 2017;10(3):187-190.
[20] Bertucci E, Giulini S, Sighinolfi G, et al. Prenatal ultrasound signs of Aarskog-Scott syndrome in a twin pregnancy: A case report. Int J Gynaecol Obstet. 2024 May;165(2):837-839.
[21] Tsukahara M, Fernandez GI. Umbilical findings in Aarskog syndrome. Clin Genet. 1994 May;45(5):260-265.
[22] Fernandez I, Tsukahara M, Mito H, et al. Congenital heart defects in Aarskog syndrome. Am J Med Genet. 1994 May 1;50(4):318-322.
[23] Nouraei SM, Hasan A, Chaudhari MP, Dunning J. Aarskog syndrome with aortic root dilatation and sub-valvular aortic stenosis: surgical management. Interact Cardiovasc Thorac Surg. 2005 Feb;4(1):47-48.
[24] Bottani A, Orrico A, Galli L, et al. Unilateral focal polymicrogyria in a patient with classical Aarskog-Scott syndrome due to a novel missense mutation in an evolutionary conserved RhoGEF domain of the faciogenital dysplasia gene FGD1. Am J Med Genet A. 2007 Oct 1;143A(19):2334-2338.
[25] van den Bergh P, Fryns JP, Wilms G, et al. Anomalous cerebral venous drainage in Aarskog syndrome. Clin Genet. 1984 Mar;25(3):288-294.
Discussion Board
Winners

Javier Cortejoso Spain Physician

Ionut Valcea Romania Physician

Le Tien Dung Viet Nam Physician

ASHLEA HARDIN United States Sonographer

ANDRES ARENCIBIA MOLINA United States Physician