Case of the Week #630
Department of Genetics Polish Mother's Memorial Hospital, Lodz, Poland
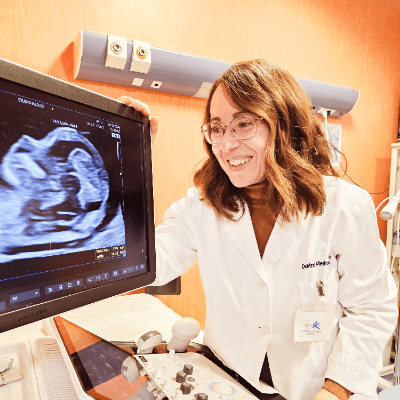
We present a case of a fetus at 19 to 20 weeks of pregnancy in a patient with non-contributory anamnesis.
View the Answer Hide the Answer
Answer
We present a case of Pfeiffer Syndrome with tympanic ring hypoplasia. Genetic amniocentesis revealed a pathogenic mutation in the FGFR2 gene.
Our ultrasound shows the typical features of Pfeiffer syndrome including premature fusion of the coronal sutures resulting in tower skull and brachycephaly, midface hypoplasia, a low nasal bridge, hypertelorism, and exophthalmos.
Discussion
Pfeiffer syndrome is a rare genetic disorder primarily characterized by craniosynostosis, a condition in which the premature fusion of skull sutures leads to distinct craniofacial and skeletal abnormalities [1]. This syndrome results from mutations in the FGFR1 or FGFR2 genes and follows an autosomal dominant inheritance pattern [2]. Clinically, Pfeiffer syndrome is classified into three subtypes, Types 1, 2, and 3, each varying in severity and associated complications [3].
- Type 1 (Classic Pfeiffer Syndrome): The mildest form, often associated with moderate craniosynostosis. Individuals generally have normal or near-normal intelligence and may experience fewer complications.
- Type 2 (Severe with Cloverleaf Skull): A more severe variant characterized by the cloverleaf skull deformity, profound neurodevelopmental impairment, and a higher likelihood of neurological and respiratory complications.
- Type 3 (Severe without Cloverleaf Skull): Similar in severity to Type 2 but without the cloverleaf skull shape. Neurological involvement remains significant, with severe developmental delays and hydrocephalus.
Craniosynostosis can affect multiple sutures, including the coronal, sagittal, lambdoid, and skull base sutures. The extent of fusion determines the skull’s shape, leading to several recognizable deformities. Brachycephaly often involves the premature fusion of the coronal sutures and describes a short and broad skull shape. Turribrachycephaly, or a "tower skull," is particularly evident in the more severe forms of Pfeiffer syndrome (Types 2 and 3) and most commonly involves premature fusion of the the coronal and sagittal sutures. The cloverleaf skull deformity (Kleeblattschädel) is a hallmark feature of Type 2, where the skull assumes a trilobed shape due to premature fusion of the coronal, sagittal, and lambdoid sutures [2,4]. In a study reviewing prenatal findings in Pfeiffer syndrome, 72% of cases identified an abnormal skull, 56% of these abnormalities were described as cloverleaf [1].
Additional skeletal abnormalities include those of the hands and feet [2]. One of its hallmark features of Pfeiffer syndrome is broad, medially deviated thumbs and great toes, which are often visibly enlarged. Individuals may also exhibit partial soft tissue syndactyly, where the fingers and toes appear partially fused. In patients with Pfeiffer syndrome, anomalies of the thumbs were identified in 33% and of the toes in 39% of prenatal ultrasounds [1].
Facial abnormalities are also prominent in individuals with Pfeiffer syndrome. A depressed nasal bridge and midface hypoplasia, a condition where the central facial bones fail to develop properly, leads to a characteristic flattened appearance [2]. Prenatally, nasal anomalies may be described as depressed nasal bridge, absent nasal bone, or nasal bone hypoplasia and is seen in 50% of cases [1]. The associated choanal stenosis and macroglossia can result in respiratory complications, potential airway obstruction and obstructive sleep apnea. Additionally, Pfeiffer and other craniosynostosis syndromes are associated with a tracheal cartilaginous sleeve where instead of distinct tracheal rings, the airway is composed of a continuous segment of cartilage, which further complicates airway management [5]. Ocular anomalies include hypertelorism and proptosis due to shallow eye sockets, which can also contribute to exposure keratopathy and potential optic nerve damage [4,6]. These findings are seen in 44% of cases prenatally [1].
Abnormalities affecting the tympanic ring and middle ear often result in conductive hearing loss, impacting auditory function. Patients with syndromic craniosynostoses such as Pfeiffer syndrome, often exhibit middle ear hypoplasia with external auditory meatus atresia or stenosis. The degree of involvement can vary depending on the specific syndrome and severity of craniofacial abnormalities [7].
The tympanic ring (also called the tympanic annulus) is a bony structure in the temporal bone that plays a crucial role in the development and support of the tympanic membrane. The tympanic ring provides a stable attachment point for the tympanic membrane, which separates the external auditory canal from the middle ear cavity. During embryonic development, the tympanic ring forms as part of the temporal bone and helps shape the middle ear cavity. Anomalies in the development of the tympanic ring can lead to malformations affecting both the external auditory canal and middle ear structures. By anchoring the tympanic membrane, the tympanic ring indirectly contributes to the efficient transmission of sound waves to the middle ear ossicles (malleus, incus, and stapes). Lebovitz et al was the first to systematically describe the prenatal assessment of tympanic rings [8]. In cases of Pfeiffer syndrome and other craniosynostoses, the tympanic ring may be hypoplastic or absent, which can result in associated middle ear abnormalities, including ossicular malformations and conductive hearing loss. Thus, hypoplasia of the tympanic ring, as seen in our case, serves as a prenatal marker for postnatal hearing loss.
Neurologically, individuals with Pfeiffer syndrome may experience hydrocephalus, particularly in Types 2 and 3, due to increased intracranial pressure. Severe forms of the condition are often associated with developmental delays and intellectual disabilities, though individuals with Type 1 may have normal or near-normal cognitive function [9].
Early identification of Pfeiffer syndrome is possible through prenatal ultrasound and genetic testing. Key ultrasound findings suggestive of the condition include abnormal skull shape due to craniosynostosis, proptosis due to shallow orbits, and limb abnormalities, particularly broad thumbs and great toes. Differential diagnosis includes other craniosynostosis syndromes such as Apert, Crouzon, and Saethre-Chotzen [1]. In cases where Pfeiffer syndrome is suspected, genetic testing can confirm the presence of FGFR1 or FGFR2 mutations, enabling early intervention, planning, and parental counseling.
References
[1] Giancotti A, D’Ambrosio V, Marchionni E, et al. Pfeiffer syndrome: literature review of prenatal sonographic findings and genetic diagnosis. J Matern Fetal Neonatal Med. 2017 Sep;30(18):2225-2231.
[2] Torres-Canchala L, Castaño D, Silva N, et al. Prenatal Diagnosis of Pfeiffer Syndrome Patient with FGFR2 C.940-1G>C Variant: A Case Report. Appl Clin Genet. 2020 Aug 11;13:147-150.
[3] Cohen MM. Pfeiffer syndrome update, clinical subtypes, and guidelines for differential diagnosis. Am J Med Genet. 1993 Feb 1;45(3):300-7.
[4] Tokumaru AM, Barkovich AJ, Ciricillo SF, et al. Skull base and calvarial deformities: association with intracranial changes in craniofacial syndromes. AJNR Am J Neuroradiol. 1996 Apr;17(4):619-30.
[5] Hockstein NG, McDonald-McGinn D, Zackai E, et al. Tracheal anomalies in Pfeiffer syndrome. Arch Otolaryngol Head Neck Surg. 2004 Nov;130(11):1298-302
[6] Clark JD, Compton CJ, Tahiri Y, et al. Ophthalmic considerations in patients with Pfeiffer syndrome. Am J Ophthalmol Case Rep. 2016 Apr 7:2:1-3.
[7] Vallino-Napoli LD. Audiologic and otologic characteristics of Pfeiffer syndrome. Cleft Palate Craniofac J. 1996 Nov;33(6):524-9.
[8] Leibovitz Z, Egenburg S, Bronshtein M, et al. Sonographic imaging of fetal tympanic rings. Ultrasound Obstet Gynecol. 2013 Nov;42(5):536-44.
[9] Mavridis IN, Rodrigues D. Nervous system involvement in Pfeiffer syndrome. Childs Nerv Syst. 2021 Feb;37(2):367-374.
Discussion Board
Winners

Javier Cortejoso Spain Physician

Andrii Averianov Ukraine Physician

Alexandr Krasnov Ukraine Physician

Andres Arencibia United States Physician

Mayank Chowdhury India Physician

Tatiana Koipish Belarus Physician

carlos lopez Venezuela Physician
CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician
Anita Silber Israel Physician

Peter conner Sweden Physician

Viorel Suciu-Lazar United States
Kimberly Delaney United States Sonographer
Marianovella Narcisi Italy Physician

Elena Andreeva Russian Federation Physician
Muradiye YILDIRIM Turkey Physician
Eti Zetounie Israel Sonographer

Sonio Sonio France AI
ANA PAULA PASSOS Brazil Physician

Ionut Valcea Romania Physician

Hien Nguyen Van Viet Nam Physician

Annette Reuss Germany Physician
Vu The Anh Viet Nam Physician

Sruthi Pydi India Physician
philip pattyn Belgium Physician

Petra Barboríková Slovakia Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician

Le Duc Viet Nam Physician

Petra Zembjakova Slovakia Physician

Hana Habanova Slovakia Physician
Dr Abhinaya Subramaniam India Physician

ASHLEA HARDIN United States Sonographer

Manuel Rodriguez Mexico Physician
ZHANNA Kurmangaliyeva Kazakhstan Physician

Dubyanskaya Yuliya Russian Federation Physician
Elvira del Rosario Cienfuegos Rojas Peru Physician