Case of the Week #628
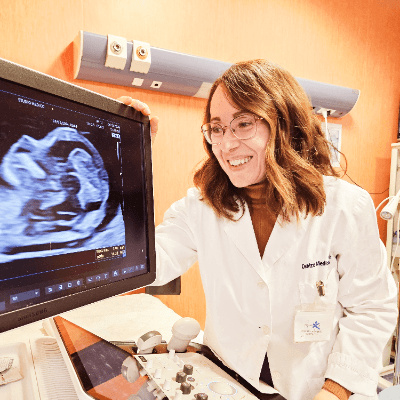
Santokba Durlabhji Memorial Hospital, Jaipur, Rajasthan
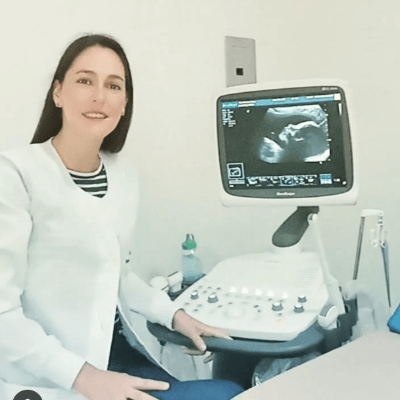
27-year-old primigravid woman presented for ultrasound evaluation at 27 weeks gestation. There was no significant family history or drug exposure during pregnancy. The following findings were observed:








View the Answer Hide the Answer
Answer
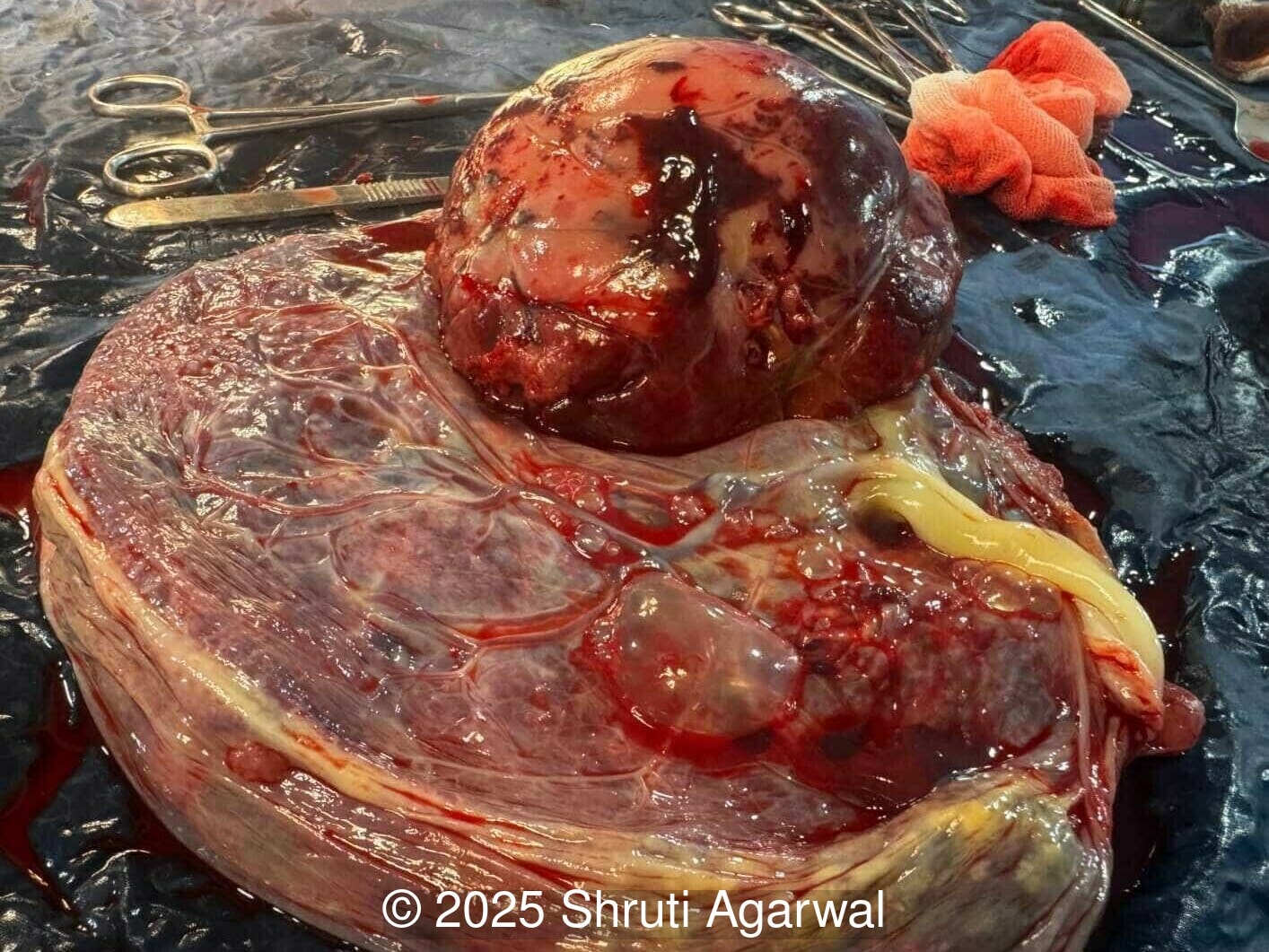
We present a case of fetal anemia due to a giant chorangioma.
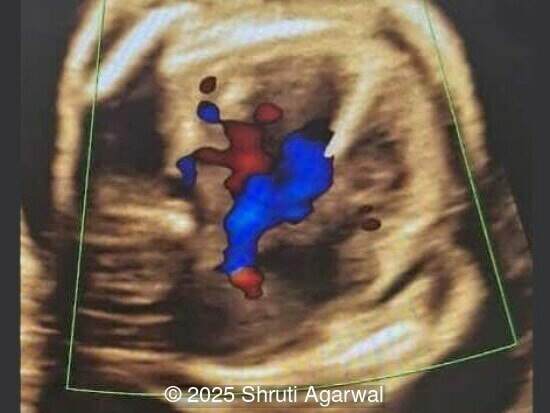
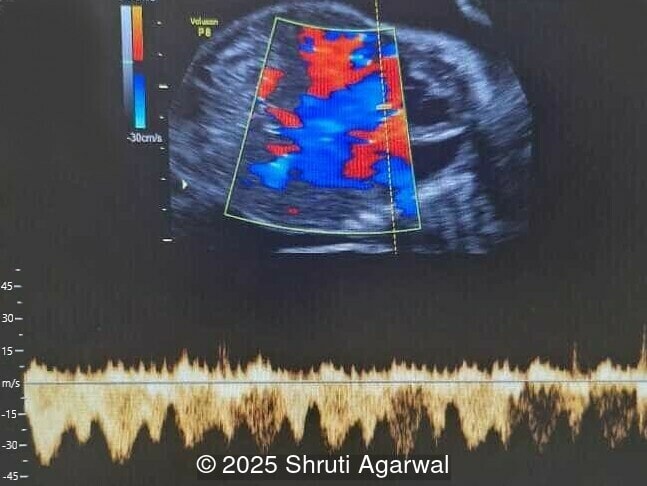
- Image 1,2: Large placental tumor is identified with internal vascularity
- Image 3: Cardiomegaly
- Image 4: pericardial effusion
- Image 5: normal cardiac inflow
- Image 6,7: Mitral regurgitation
- Image 8: Normal ductus venosus
- Image 9: Middle cerebral artery peak systolic velocity >1.5MOM suggesting fetal anemia
- Image 10: polyhydramnios
No other fetal structural anomalies were found and there were no pregnancy complications. The patient was counselled regarding fetal laser treatment of the chorangioma however the family was from a rural area and the treatment was not accessible or affordable for them. Due to the fetal cardiac changes, the patient was delivered by caesarean section at 28 weeks. The diagnosis was confirmed after birth. The infant was treated in the neonatal intensive care unit and transfused one unit of blood with postnatal resolution of the cardiac findings.

Discussion
Placental chorangioma is the most common neoplasm of the placenta occurring in approximately 0.6% of all pregnancies [1]. In most cases, the tumor is less than 5cm in size and asymptomatic [2]. Chorangioma is considered a hamartoma or hyperplastic capillary lesion rather than a true neoplasm due to its inability to metastasize, and the tumor has no malignant potential [3]. Chorangiomas are usually found in the third trimester as a solitary nodule in the placental parenchyma. On gross examination, the chorangioma is well-circumscribed, without a fibrous capsule, and sharply demarcated from the surrounding placental parenchyma by a single or double layer of chorionic epithelium. It tends to have fleshy, congested, red to tan colored surface [4]. The most common location is in the fetal surface of the placenta, in proximity of the umbilical cord insertion. A larger tumor is usually attached to the chorion, which is a less perfused area. A few cases have been reported on the maternal surface, replacing the whole or some part of the placental lobe [4,5]. Chorangiomas tend to arise in areas of hypoperfusion. A hypoxic state is thought to lead to active proliferation of connective tissue and growth of villous capillaries mediated by vascular growth factors [6]. Pre-eclampsia, high-altitude, and fetal anemia have been associated with chorangioma, suggesting that decreased oxygen tension may play a role in the pathogenesis [7,8].
Chorangiomas greater than 5cm are referred to as a giant chorangioma and occur in approximately 1 in 2,700 pregnancies [2]. Giant chorangioma can be clinically significant, causing various fetomaternal complications. In a study reviewing 175 cases of chorangioma, approximately 34% of giant chorangiomas experienced complications [2]. Arteriovenous shunting in giant chorangioma can increase venous return to the fetal heart, causing hypervolemia, tachycardia, and cardiomegaly, leading to heart failure, hydrops fetalis, and fetal demise. Large lesions can also divert nutrients and oxygen from the fetus, manifesting as growth restriction. Placentomegaly occurs due to a hyperdynamic circulation as a result of arteriovenous shunting. In such cases, fetus may suffer from anemia and thrombocytopenia due to sequestration of red blood cells and platelets by the tumor. Polyhydramnios can occur due to both direct transudation into the amniotic fluid and to fetal polyuria secondary to the hyperdynamic circulation. Additionally, preterm delivery and maternal mirror syndrome with generalized fluid overload and preeclampsia can occur with giant chorangiomas [2,8].
Prenatal diagnosis depends on ultrasound, however, chorangioma can cause an increase in maternal serum alpha-fetoprotein [3]. Ultrasound examination reveals a hypo- or hyperechoic, well-circumscribed mass, which is usually located underneath the chorionic plate near the umbilical cord insertion, and often protrudes into the amniotic cavity. Color Doppler demonstrates large vascular channels around and within the tumor [6,9]. In cases of giant chorangiomas, echocardiography should be performed to assess cardiac function and measure fetal middle cerebral artery peak systolic velocity for diagnosis of fetal anemia. Regular ultrasounds with Doppler studies are used to monitor tumor size, fetal growth, amniotic fluid volume, and signs of fetal anemia or heart failure. The frequency of exams is based on tumor size and associated complications. With small tumors, assessment may occur every 3-4 weeks, whereas in large tumors, the ultrasound scan may be done every 1-2 weeks [3]. These regular assessments can diagnose conditions that require intervention, such as polyhydramnios, hydrops, or hemolytic anemia.
Several interventions have been performed for pregnancies with complicated giant chorangioma and include endoscopic surgical devascularization, fetal transfusion for correcting anemia, chemosclerosis using absolute alcohol, and fetoscopic laser coagulation [3]. Therapeutic amniocentesis or maternal indomethacin therapy may be indicated for polyhydramnios. Early delivery may be recommended if there is evidence of poor growth, fetal hypoxia or hydrops. In pregnancies delivered preterm, steroid administration for fetal lung maturity acceleration can optimize postnatal outcomes [9].
Besides the histopathology examination, ultrasonography and particularly color Doppler sonography is helpful in differentiating chorangioma from other placental pathologies such as hematoma, infarcts, intervillous thrombosis, partial mole, leiomyoma, and placental teratoma. The pattern of blood flow to the tumor can assist in differentiating between different placental tumors [3,10].
Prognosis depends on the size of the tumor and associated maternal and fetal complications. Symptomatic giant chorioangiomas carry a higher risk of mortality at approximately 18% [2]. There is no increased risk of recurrence.
References
[1] Guschmann M, Henrich W, Entezami M. Chorioangioma--new insights into a well-known problem. I. Results of a clinical and morphological study of 136 cases. J Perinat Med. 2003;31(2):163-9.
[2] Ma H, Liu Z, Ruan J. Placental chorioangioma and pregnancy outcome: a ten-year retrospective study in a tertiary referral centre. BMC Pregnancy Childbirth. 2023 May 25;23:381.
[3] Ruman U, Chowdhury TS, Nessa M. Placental chorioangioma: a case report and review. Birdem Med J. 2012 Oct;2(2):113-115.
[4]. Lež C, Fures R, Hrgovic Z, et al. Chorangioma placentae. Rare Tumors. 2010 Dec 31;2(4):e67.
[5] Ingale YP, Buch AC, Ulhas PN, et al. Incidental Detection of Chorangioma with Chorangiosis of Placenta: A Rare Case Report. Med J Dr DY Patil Visyapeeth. 2019 Mar;12(2):174-176.
[6] Akbarzadeh-Jahromi M, Soleimani N, Mohammadzadeh S. Multiple chorangioma following long-term secondary infertility: A rare case report and review of pathologic differential diagnosis. Int Med Case Rep J. 2019 Dec;19(12):383-387.
[7] Mohammed U, Mohammmed A, Jimoh AO, et al. Placental Chorangioma. Sahel Med J. 2018;21(2):113-115.
[8] Dong T, Sher D, Luo Q. Pregnancy complications and adverse outcomes in placental chorioangioma: a retrospective cohort analysis. J Matern Fetal Neonatal Med. 2020 Jul;33(13):2269-2273.
[9] Kodandapani S, Shreshta A, Ramkumar V, et al. Chorioangioma of Placenta: A Rare Placental Cause for Adverse Fetal Outcome. Case Rep Obstet Gynecol. 2012 Jun 13;2012:913878.
[10] Sepulveda W, Aviles G, Carstens E, et al. Prenatal diagnosis of solid placental masses: the value of color flow imaging. Ultrasound Obstet Gynecol. 2000 Nov;16(6):554-8.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Padman KG United Kingdom Sonographer

Pawel Swietlicki Poland Physician

Chursina Olga Russian Federation Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician

Vera Osadshaya Russian Federation Physician

Vladimir Lemaire United States Physician
Ivan Ivanov Russian Federation Physician
Boujemaa Oueslati Tunisia Physician

carlos lopez Venezuela Physician

Aysegul Ozel Turkey Physician

Rushina Patel United States Sonographer
Caroline Reichert Garcia Brazil Physician

Olivia Ionescu United Kingdom Physician
Marianovella Narcisi Italy Physician

ARAVIND NARAVULA India Physician

CHEN YANG China Physician
Amparo Gimeno Spain Physician

Elena Andreeva Russian Federation Physician

Muradiye YILDIRIM Turkey Physician

Miguel Merino United States Physician

CRISTINA MARTINEZ PAYO Spain Physician

ALBANA CEREKJA Italy Physician
Eti Zetounie Israel Sonographer

Deval Shah India Physician

SAMUEL GELVEZ TELLEZ Colombia Physician

Murat Cagan Turkey Physician
ANA PAULA PASSOS Brazil Physician

Ionut Valcea Romania Physician

Sviatlana Akhramovich Belarus Physician
Đặng Mai Quỳnh Viet Nam Physician

Halil Korkut Dağlar United States Physician

Elham Eghbali Iran, Islamic Republic of Radiologist

Hien Nguyen Van Viet Nam Physician

Kathrine Montagne United States Sonographer

Miguel Sanchez Mexico Physician

Kareem Haloub Australia Physician
Zuzana Briešková Slovakia Physician

Subapriya Kandasamy India Physician

András Weidner Hungary Physician

SILVIO SHIGETOMI Brazil Physician

Ann-Christin Dr. Sönnichsen Germany Physician
Fred Pop Uganda Sonographer

Annette Reuss Germany Physician
Jay Vaishnav India Physician
CHERYL TURNER United States Sonographer

Nguyen Xuan Cong Viet Nam Physician

Laura Wharton United Kingdom Physician

zozo sichala Zambia radiology technologist

Shina Kaur India Physician

Denys Saitarly Israel Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician

Costin Radu Lucian Romania Physician

Seval Yılmaz Ergani Turkey Physician

María Victoria Peral Parrado Spain Physician

Margarita Gallardo Arozena Spain Physician

Le Duc Viet Nam Physician

Hana Habanova Slovakia Physician

Dr Mayur C Trivedi India Physician

Gnanasekar Periyasamy India Physician
Rhaiza Urbina Venezuela Medico Materno Fetal
Navya Sri Mopada India Physician

Katsiaryna Adamenko France Physician

CARLOS JOSE PIÑA VILLEGAS Peru Physician

ASHLEA HARDIN United States Sonographer

Victor Hugo Ribeiro Brazil Physician

Sidharthan S India Physician

Ali Ozgur Ersoy Turkey Physician

Gökçen Örgül Turkey Physician
Manuel Rodriguez Mexico Physician
ZHANNA Kurmangaliyeva Kazakhstan Physician

Reshma Marineni India Physician
Crystal Eskew United States Sonographer

Shyamala Ramesh India Physician
VINUTHA REDDY PASHAM India Physician

Surekha Bhimangouda India Physician

Charmi Prajapati India Sonographer

Narmada Damodaran India Physician

RAVINDRANATH MALLELA India RADIOLOGIST

Giovanna Contratti Italy Physician

Albert Guarque Rus Spain Physician

Sergey Shumakov Russian Federation Physician