Case of the Week #625
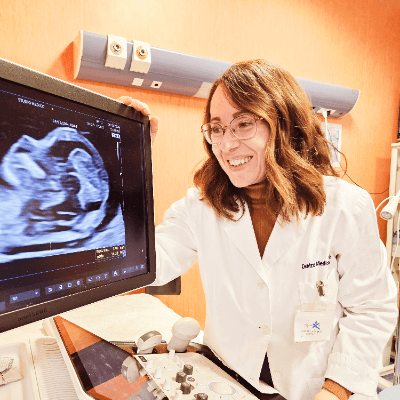
(1) Monash Ultrasound for Women, Melbourne, Australia; (2) UCSF Health, San Francisco, California, USA
40-year-old G2P1 woman without significant medical history presents for routine first trimester screening at 13 weeks. Her first pregnancy was unremarkable. The following findings were observed:



View the Answer Hide the Answer
Answer
We present a case of open spina bifida diagnosed in the first trimester. Parents opted for termination.
Our images demonstrated early changes in the midbrain that prompted a targeted investigation of the fetal spine, which revealed a lumbo-sacral defect.
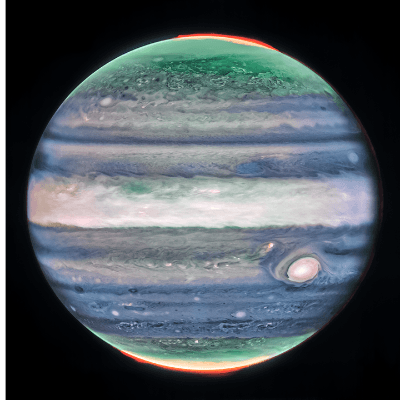
- Image 1: Transverse section of the brain at the level of choroids. Subtle supporting sign of relatively large choroid plexuses and low surrounding cerebrospinal fluid known as the "dry brain" sign.
- Image 2: Transverse section of the brain at the level of the aqueduct of Sylvius. Midbrain is seen juxtaposed to the occiput, known as "crash" sign.
- Image 3, Video 1: Mid-sagittal image demonstrating the mid brain and brain stem displaced posteriorly, known as the "crash" sign. Intracranial translucency is difficult to visualize.
- Video 2: Sagittal video of the spine showing a subtle skin defect in the area of the anomaly.
- Video 3: Transverse video of the spine showing more obvious open spinal defect in lumbo-sacral region.


Discussion
Spina bifida, a neural tube defect resulting from incomplete closure of the spinal cord and surrounding structures, is a condition with significant clinical implications. Advances in prenatal screening and diagnostic imaging have led to improved early detection, particularly through sonographic assessment. We explore the sonographic features of spina bifida, focusing on early detection methods in the first and second trimesters and their diagnostic significance for sonographers.
Open spina bifida is commonly associated with Arnold-Chiari II malformation, a condition caused by cerebrospinal fluid (CSF) leakage into the amniotic cavity, leading to hypotension in the subarachnoid space. This results in caudal displacement of the brainstem and obliteration of the cisterna magna. As a consequence, a range of intracranial and spinal abnormalities manifest on ultrasound, providing crucial diagnostic clues. The first-trimester ultrasound, performed between 11 and 14 weeks, presents an opportunity for early detection of spina bifida using various indirect cranial markers. Several key signs have been described:
1. Intracranial translucency (IT) represents the fourth ventricle, which appears as a hypoechoic space in the mid-sagittal view of the fetal face. In open spina bifida, intracranial translucency may be absent or compressed due to Arnold-Chiari II malformation [1].


2. Brainstem and Brainstem-Occipital Bone (BSOB) Distance measurements can suggest the diagnosis of open spina bifida. An increased brainstem diameter with reduced BSOB distance results in an elevated BS:BSOB ratio, which is a reliable indicator of open spina bifida. In fetuses with open spina bifida compared to normal fetuses, the brain stem diameter (BS) is higher, the BSOB diameter is lower resulting in an increased BS:BSOB ratio [2].


3. A reduction in the Frontomaxillary Facial Angle can be seen in fetuses with open spina bifida as these cases often show a narrower frontomaxillary facial angle due to altered intracranial pressure dynamics. The angle is measured from a line along the upper surface of the palate, and a line that traverses the anterior aspect of the maxilla extending to the external surface of the forehead [3].


4. Dry Brain Sign is characterized by an exaggerated size of the choroid plexuses filling the lateral ventricles due to diminished cerebrospinal fluid in the ventricular system. Unidirectional leakage of fluid towards the open spinal defect results from a pressure gradient between the “high-pressure” CSF-filled choroid ventricles and, “low-pressure” spinal cord, which produces posterior and caudal displacement of the mesencephalon. As a result, the reduced fluid in the lateral ventricles causes the choroid plexuses to fill the cranial cavity [4-5].


5. The Crash Sign describes the posterior displacement and deformation of the mesencephalon against the occipital bone due to reduced intracranial pressure caused by cerebrospinal fluid leakage. This is a promising early marker seen in a majority of first-trimester open spina bifida cases. During this posterior displacement, the mesencephalon meets the only firm cranial structure on its way, the occipital bone, and is compressed against it. On mid-sagittal view the brainstem is thickened and shifted posteriorly [6].


By the second trimester (18-22 weeks), spina bifida can be more definitively diagnosed using characteristic cranial and spinal abnormalities:
- Lemon Sign describes the indentation of the frontal bones due to reduced intracranial pressure and is reported in ~98% of cases before 24 weeks but decreases in frequency later in gestation [7].
- Banana Sign is identified when the cerebellum appears curved and elongated due to downward displacement, replacing the normal round shape. This finding is present in 72-81% of cases [7].
- Ventriculomegaly describes the enlargement of the lateral ventricles due to obstructive hydrocephalus secondary to Arnold-Chiari II malformation.
- Direct spinal examination can identify disruption of the normal ossification pattern, with widening or discontinuity of the posterior elements. There may be a cystic or solid mass at the site of the lesion.


Sonographers play a crucial role in the early detection of spina bifida. Recognizing first-trimester cranial markers allows for early suspicion and targeted spinal examination. The key recommendations include a routine mid-sagittal brain examination in which the posterior brain structures are always assessed in the standard nuchal translucency view. Additionally, the intracranial translucency visibility is recorded and the BS/BSOB ratios are measured when abnormalities are suspected. Secondly, a targeted axial head and spine view should include a detailed axial plane assessment for ventriculomegaly and dry brain sign in cases with suspected open spina bifida. Spinal integrity should be confirmed in three orthogonal planes. If visualization is suboptimal, consider a follow-up scan in 2-3 weeks to reassess cranial and spinal structures. Additionally, transvaginal ultrasound may enhance visualization, particularly in early gestation.
In conclusion, early detection of spina bifida on ultrasound relies on identifying characteristic cranial and spinal abnormalities. First-trimester screening offers an opportunity for early suspicion, while second-trimester imaging provides definitive diagnosis. By incorporating standardized assessment protocols and recognizing novel sonographic markers, sonographers can improve diagnostic accuracy, facilitating timely intervention and comprehensive prenatal counseling for affected pregnancies.
References
[1] Chaoui R, Benoit B, Mitkowska-Wozniak H, et al. Assessment of intracranial translucency (IT) in the detection of spina bifida at the 11–13-week scan. Ultrasound Obstet Gynecol. 2009 Sep;34(3):249-52.
[2] Lachmann R, Chaoui R, Moratalla J, et al. Posterior brain in fetuses with open spina bifida at 11 to 13 weeks. Prenat Diagn. 2011 Jan;31(1):103-6.
[3] Lachmann R, Picciarelli G, Moratalla J, et al. Frontomaxillary facial angle in fetuses with spina bifida at 11–13 weeks' gestation. Ultrasound Obstet Gynecol. 2010 Sep;36(3):268-71.
[4] Chaoui R, Benoit B, Entezami M, et al. Ratio of fetal choroid plexus to head size: simple sonographic marker of open spina bifida at 11-13 weeks' gestation. Ultrasound Obstet Gynecol. 2020 Jan;55(1):81-86.
[5] Kalafat E, Ting L, Thilaganathan B, et al. Diagnostic accuracy of fetal choroid plexus length to head biometry ratio at 11 to 13 weeks for open spina bifida. Am J Obstet Gynecol. 2021 Mar;224(3):294.e1-294.e14.
[6] Ushakov F, Sacco A, Andreeva E, et al. Crash sign: new first-trimester sonographic marker of spina bifida. Ultrasound Obstet Gynecol. 2019 Dec;54(6):740-745.
[7] Van den Hof MC, Nicolaides KH, Campbell J, et al. Evaluation of the lemon and banana signs in one hundred thirty fetuses with open spina bifida. Am J Obstet Gynecol. 1990 Feb;162(2):322-7.
Discussion Board
Winners

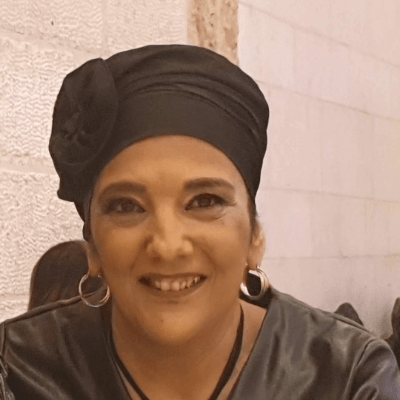
Zhanna Bondarchuk Ukraine Physician

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Pawel Swietlicki Poland Physician

Chursina Olga Russian Federation Physician

belen garrido Spain Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician

Olha Petrenko Ukraine Physician

Gayatri K India Physician

Nutan Thakur India Physician

Vladimir Lemaire United States Physician
Ivan Ivanov Russian Federation Physician

Boujemaa Oueslati Tunisia Physician

carlos lopez Venezuela Physician

Aysegul Ozel Turkey Physician
Anita Silber Israel Physician

Oleg Vinogradov Russian Federation Physician

Rabeb Mouelhi Germany Physician

Panagiotis Benardis Greece Physician
Kimberly Delaney United States Sonographer

Olivia Ionescu United Kingdom Physician
Marianovella Narcisi Italy Physician

Elena Andreeva Russian Federation Physician

Muradiye YILDIRIM Turkey Physician

Quan Kun China Physician

Ta Son Vo Viet Nam Physician

ALBANA CEREKJA Italy Physician
Eti Zetounie Israel Sonographer

Deval Shah India Physician

Amaal Asad United States

Murat Cagan Turkey Physician

Laurie Briare United States Sonographer
Büşra Cambaztepe Turkey Physician

gholamreza azizi Iran, Islamic Republic of Physician

Ionut Valcea Romania Physician

Sviatlana Akhramovich Belarus Physician

Đặng Mai Quỳnh Viet Nam Physician

Halil Korkut Dağlar United States Physician

Hien Nguyen Van Viet Nam Physician

Miguel Sanchez Mexico Physician

Almaz Kinzyabulatov Russian Federation Physician

Kareem Haloub Australia Physician

Vitor Oliveira Brazil Physician

Zuzana Briešková Slovakia Physician

Katarína Pitoňáková Czech Republic Physician

András Weidner Hungary Physician

Maria Kuznetsova Russian Federation Physician
Fred Pop Uganda Sonographer

Annette Reuss Germany Physician

Arati Appinabhavi India Physician
shruti Agarwal India Physician
Vu The Anh Viet Nam Physician
Jay Vaishnav India Physician
CHERYL TURNER United States Sonographer

Nguyen Xuan Cong Viet Nam Physician

Perrine Riou-Kerangal French Polynesia Sage-femme échographiste

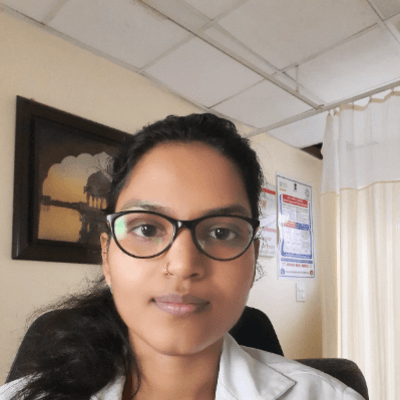
Poojitha Alladi India Physician
shay kevorkian Israel Physician

Sruthi Pydi India Physician

Rupal Sasani India Physician

Claudio Luna Venezuela Physician

Carmen de Luis Rodríguez Spain Physician

Viveka S M India Physician

Denys Saitarly Israel Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician

Kobie Golledge Australia Sonographer

Costin Radu Lucian Romania Physician

Zina Kerbi Algeria Physician

María Victoria Peral Parrado Spain Physician

Zeynep Seyhanli Turkey Physician

Volha Smal Poland Physician

Le Duc Viet Nam Physician

Gulira Turumbekova Kyrgyzstan Physician

PADMA Priya DHARSHINI India Physician

Hana Habanova Slovakia Physician

Tamara Yarygina Russian Federation Physician

Anjali Gupta India Physician
Marius Bogdan Muresan Romania Physician

Elena Ivanova-Tosheva Bulgaria Physician

Gnanasekar Periyasamy India Physician
Jagdish Suthar India Physician

José Velasco Ecuador Physician

Severina Gesheva United States Sonographer

Hân Đỗ Viet Nam Physician

CARLOS JOSE PIÑA VILLEGAS Peru Physician

zhong xiaoyan China Physician

Yugandhara Kamble India Physician

Ali Ozgur Ersoy Turkey Physician

Ayse Ceren Duymus Turkey Physician

Gökçen Örgül Turkey Physician

Neha Gupta India Physician

Manuel Rodriguez Mexico Physician
ZHANNA Kurmangaliyeva Kazakhstan Physician

Liam McCullough Slovakia Physician

Reshma Marineni India Physician

madhavilatha routhu India Physician

Shyamala Ramesh India Physician

ahmad ali davar Iran, Islamic Republic of Physician

mayank hariyani India Sonographer
Mukesh Kannan India Consultant radiologist

yujia mao United States Physician

Dubyanskaya Yuliya Russian Federation Physician

Olga Gundareva Russian Federation Physician

Trilokesh Patra India Radiologist