Case of the Week #620
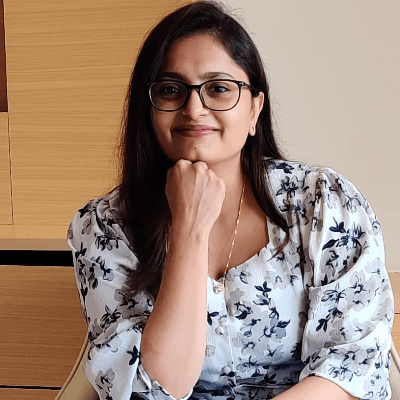
Sanjeevani Sonography Centre, Hanumangarh, Rajasthan
A 25-year-old G2P1 woman presented for a routine fetal ultrasound at 25 weeks gestation. The patient had no significant past medical history, and her first pregnancy was unremarkable.





View the Answer Hide the Answer
Answer
We present a case of fetal TORCH infection causing pathologic pericholecystic calcifications and fetal hydrops. Testing was positive for Herpes Simplex Virus infection. Intra-uterine fetal death was observed at 30 weeks of gestation.
Parameter | Value | Unit | Interpretation | Biological Reference Range |
|---|---|---|---|---|
IgG: Immunoglonbulin G, CMV: Cytomegalovirus, HSV: Herpes Simplex Virus | ||||
Toxoplasma IgG | 0.01 | IU/mL | Negative | <2.0 Negative, >2.0 Positive |
Rubella virus IgG | 0.02 | AU/mL | Negative | <2.0 Negative, >2.0 Positive |
CMV IgG | 2.82 | AU/mL | Negative | <2.0 Negative, >2.0 Positive |
HSV 1&2 IgG | 27.70 | Index Value | Positive | <2.0 Negative, >2.0 Positive |
Our ultrasound images demonstrated moderate fetal ascites, significant right-sided pleural effusion with mediastinal shift, minimal left-sided pleural effusion, and calcifications around the fetal gallbladder.
- Video 1, Image 1: Moderate ascites observed within the fetal abdomen, characterized by free fluid accumulation in the peritoneal cavity.
- Video 1, Image 2: Significant right pleural effusion noted, causing a mediastinal shift towards the left side. Minimal pleural effusion in the left chest.
- Image 3: Few calcifications were observed around the fetal gallbladder which also had a hyperechoic wall, suggesting the possibility of intra-abdominal infection.
- Image 4: Fetal umbilical artery doppler
- Image 5: Ductus venosus doppler
Discussion
The findings of moderate fetal ascites, significant right-sided pleural effusion with a left-sided mediastinal shift, and calcifications around the fetal gallbladder are concerning for potential non-immune hydrops fetalis or underlying congenital or infectious pathology. Our differential diagnosis included the following:
- Fetal infections (TORCH): Calcifications around the gallbladder may suggest intrauterine infections, such as cytomegalovirus or toxoplasmosis [1], which can lead to fetal hydrops.
- Fetal Hydrops: Non-immune hydrops fetalis should be considered due to the presence of both pleural effusion and ascites. Potential causes may include fetal anemia, cardiovascular anomalies, infections (such as cytomegalovirus or toxoplasmosis), and chromosomal abnormalities [4,5].
- Congenital Diaphragmatic Hernia (CDH): Although typically associated with left-sided pleural effusion, CDH can present atypically. The mediastinal shift may indicate significant effusion rather than herniation.
Hydrops fetalis occurs in 1.3 to 1.8 in 1000 [2,3] and can be caused by cardiac disorders, genetic abnormalities, fetal malformations, hematologic disorders and infections [4,5]. Nonimmune fetal hydrops accounts for 80% while Rhesus incompatibility accounts for the remaining 20% of cases [2]. Mortality from fetal hydrops is high and depends on the etiology and gestational age at diagnosis [2,6]. In fetuses with hydrops, approximately 10-15% are caused by intrauterine infection [5-7]. The most common infectious causes are cytomegalovirus, toxoplasmosis, syphilis, and parvovirus B19. Herpes Simplex Virus (HSV) is rarely described as a cause of fetal hydrops. Pfister et al performed a literature review and found only five cases of fetal hydrops caused by HSV [4].
In a review of Chinese population over a 5-year period, the hospitalization rate due to congenital TORCH infections was approximately 18 per 100,000 hospitalized neonates and 5% were affected with HSV [8]. Most cases of neonatal HSV infections occur from exposure to the virus in the genital tract during delivery, though only one-third of mothers have genital or oral lesions during pregnancy [9]. Mothers with a first clinical genital herpes episode have a much higher risk for transmission of the virus to the fetus than mothers with recurrent infections [10].
It is estimated that intrauterine infection occurs in 4-5% of neonatal HSV cases [11]. Infants infected with HSV in utero typically have a triad of clinical findings including cutaneous manifestations (hypopigmented scar, erosion, ulceration, or vesiculobullous lesions), ophthalmologic findings (microopthalmia, keratitis, or chorioretinitis), and neurologic involvement (microcephaly, ventriculomegaly, encephalomalacia, or intracranial calcification) [4,9,11]. Marquez et al review 64 intrauterine HSV cases and found that cutaneous lesions were the most common manifestation while the triad of cutaneous, central nervous system and ophthalmologic disease occurred in 30% of cases. Additionally, they found that one-third of cases had visceral involvement, presenting most commonly as liver disease with hepatomegaly, elevated transaminases, or hepatic calcifications. Postmortem examination of infants with intrauterine HSV infection revealed necrosis of the liver, adrenals, or lungs as well as dystrophic calcification in the brain, adrenals, and liver. Prematurity affected 64% of infants. Nearly 10% of cases had hydrops and all cases of hydrops were fatal. Almost half (45%) of the neonates did not survive, and of the survivors, 37% had developmental delay. As a result, Marquez et al conclude that prematurity, visceral involvement, altered fetal growth, hydrops, and intrauterine demise are part of the clinical spectrum of intrauterine HSV infection [9].
In fetuses presenting with hydrops, further investigations including fetal MRI, targeted fetal echocardiography, and possible amniocentesis for karyotyping and TORCH screening, are recommended to elucidate the etiology and guide management. Regular follow-up with serial ultrasounds can clarify the prognosis and plan appropriate management of the pregnancy and delivery. Additionally, a multidisciplinary approach involving neonatology, pediatric surgery, and pediatric infectious disease specialists can facilitate delivery planning and postnatal care.
References
[1] Simchen MJ, Toi A, Bona M, et al. Fetal hepatic calcifications: prenatal diagnosis and outcome. Am J Obstet Gynecol . 2002 Dec;187(6):1617-22.
[2] Trainor B, Tubman R. The Emerging Pattern Of Hydrops Fetalis - Incidence, aetiology and management. Ulster Med J. 2006 Sep;75(3):185–186.
[3] Ratanasiri T, Komwilaisak R, Sittivech A, et al. Incidence, causes and pregnancy outcomes of hydrops fetalis at Srinagarind Hospital, 1996-2005: a 10-year review. J Med Assoc Thai. 2009 May;92(5):594-9.
[4] Pfister KM, Schleiss MR, Reed RC, et al. Non-immune hydrops fetalis caused by herpes simplex virus type 2 in the setting of recurrent maternal infection. J Perinatol. 2013 Oct;33(10):817-20.
[5] Miriam Morey-Olivé M, Marín Córdoba C, Camba Longueira F, et al. Neonates with a prenatal diagnosis of hydrops fetalis: A 10-year experience in a tertiary care center. An Pediatr (Engl Ed). 2024 Feb;100(2):115-122.
[6] Sileo FG, Kulkarni A, Branescu I, et al. Non-immune fetal hydrops: etiology and outcome according to gestational age at diagnosis. Ultrasound Obstet Gynecol. 2020 Sep;56(3):416-421.
[7] Sohan K, Carroll SG, De La Fuente S, et al. Analysis of outcome in hydrops fetalis in relation to gestational age at diagnosis, cause and treatment. Acta Obstet Gynecol Scand. 2001 Aug;80(8):726-30.
[8] Zhang L, Wang X, Liu M, et al. The epidemiology and disease burden of congenital TORCH infections among hospitalized children in China: A national cross-sectional study. PLoS Negl Trop Dis. 2022 Oct 14;16(10):e0010861.
[9] Marquez L, Levy ML, Munoz FM, et al. A Report of Three Cases and Review of Intrauterine Herpes Simplex Virus Infection. Pediatr Infect Dis J. 2011 Feb;30(2):153–157.
[10] Brown ZA, Vontver LA, Benedetti J, et al. Effects on infants of a first episode of genital herpes during pregnancy. N Engl J Med. 1987 Nov 12;317(20):1246-51.
[11] Hutto C, Arvin A, Jacobs R, et al. Intrauterine herpes simplex virus infections. J Pediatr. 1987 Jan;110(1):97-101.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Oscar Hernández United States

Vicente Patiño Oleaque Spain Physician

Deval Shah India Physician

Ionut Valcea Romania Physician
Fred Pop Uganda Sonographer

Sruthi Pydi India Physician

Denys Saitarly Israel Physician

Tetiana Ishchenko Ukraine Physician
Hetal Patel India Physician
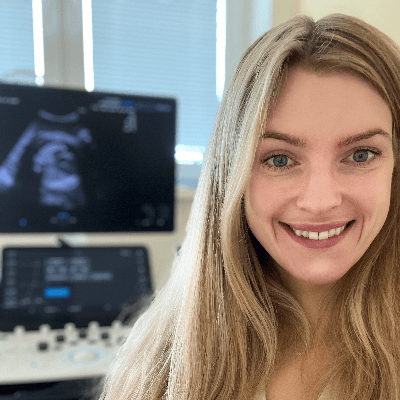
Zuzana Rak Slovakia Physician

Petra Zembjakova Slovakia Physician

Hana Habanova Slovakia Physician
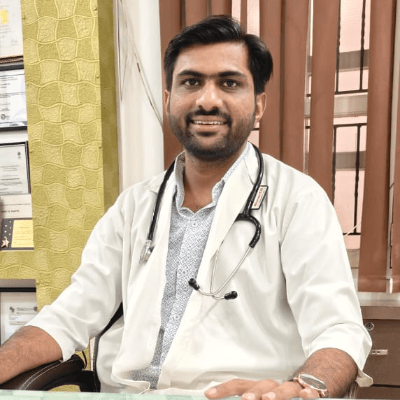
Jagdish Suthar India Physician

Sidharthan S India Physician

Tessa Meuleman Netherlands Sonographer

Gökçen Örgül Turkey Physician

Megan Garcia United States Sonographer