Case of the Week #616
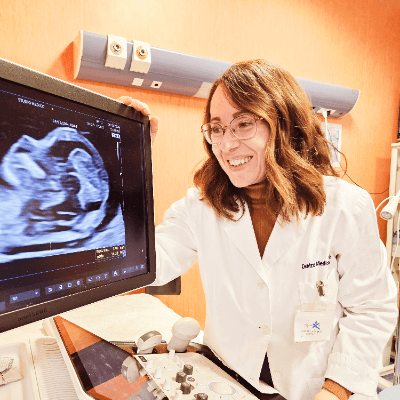
(1) Clínica Lancet, Mexico; (2) UCSF Health, San Francisco, California USA




View the Answer Hide the Answer
Answer
We present a case of bifid scrotum and hypospadias. Postnatal karyotype was normal.
Our images revealed the following findings:
- Image 1: Axial view of the fetal undifferentiated genitalia with separated genital folds. The male gonads can be partially seen and the undifferentiated genital tubercle is visible between the folds.
- Image 2: Demonstrates the separated genital folds with male gonads. The genital tubercle corresponds to a penis. Here we also see the Tulip sign, which is a clue to the diagnosis of Hypospadias.
- Image 3: Axial view of genitalia with separated genital folds corresponding to the bifid scrotum.
- Image 4: The male gonads are visible in the scrotum.


Discussion
Bifid scrotum is a midline cleft in the scrotum resulting from incomplete fusion of the labioscrotal folds during fetal development [1]. Hypospadias is a developmental anomaly in which the urethra opens on the ventral side of the penis [2]. It is the most common congenital defect of the genitalia with a prevalence of approximately 21 in 10,000 births [3]. Bifid scrotum is often associated with hypospadias and cryptorchidism, and may be a mild presentation of a disorder of sexual development. In a study reviewing 110 subjects with bifid scrotum, 86% had severe hypospadias, 31% had orchidopexy for unilateral or bilateral undescended testes [1]. Additionally, nearly 40% of cases with bifid scrotum can have additional non-genitourinary abnormalities including cardiac, neurodevelopmental, growth, neurologic, ano-rectal malformations, musculoskeletal, renal, otolaryngologic, endocrinologic, and ophthalmologic [1]. Fetuses with bifid scrotum tended to deliver preterm at an average gestational age of 35.9 weeks [1].
In the early stages of organogenesis, three basic structures are formed: the bipotential gonads, mesonephric cords, and undifferentiated external genitalia. The presence of the SRY gene on the Y chromosome initiates male sex determination. Testosterone production results in the differentiation of the gonads to testicles. The mesonephric cords form the epididymis, vas deferens and seminal glands, and the external genitalia masculinize with elongation of the phallus to form the penis, and fusion of the labioscrotal folds to form the scrotum. Testicular migration begins in the 8th week of gestation in two phases: from the 10th to the 15th week, Leydig cells produce insulin-like hormone resulting in the downward trajectory of the testicles within the abdomen due to traction exerted by the gubernacular bulb anchored in the scrotum. In the second stage, the testicles begin travelling to the scrotum around at 24th to 25th week gestation and ends at 32nd to 33rd week in 97% of fetuses [4,5].
The scrotum and genitals are not routinely evaluated by ultrasound except to establish fetal sex. As the testicles do not descend into the scrotum until approximately the 24th week of gestation, they are not routinely evaluated during the midtrimester ultrasound [4]. Abnormalities of the genitalia are more commonly identified during a detailed ultrasound examination due to the detection of other anomalies, a relevant family history, or a discrepancy between the fetal karyotype and the appearance of the external genitalia [6]. Bifid scrotum and hypospadias can be diagnosed on prenatal ultrasound, though hypospadias is often missed [2]. Ultrasound findings suggesting hypospadias include a bulbous tip of the penile shaft, ventral curvature of the penis or chordee which results from a fibrous band occurring in the projected course of the urethra, a small penile shaft with two echogenic lines corresponding to the dermal remains of the prepuce, ventral deflection of the urinary stream during micturition, and penoscrotal transposition [7]. Meizner et al described the “tulip sign” for in utero diagnosis of severe hypospadias characterized by a ventrally curved penis located within a bifid scrotum [8].
Bifid scrotum and hypospadias can be a mild presentation of a disorder of sexual development, which varies in phenotype from mild to ambiguous genitalia to sex reversal [1]. Recent studies have suggested that these milder cases of undervirilization presenting with hypospadias, bifid scrotum or cryptorchidism have underlying genetic mutations in Androgen Receptor (AR), Nuclear Receptor Subfamily 5 Group A Member 1 (NR5A1), Wilms Tumor 1 (WT1) and steroid 5a-reductase type 2 (SRD5A2) genes [9-12]. In a study reviewing 110 subjects with bifid scrotum, of the patients who had any type of genetic testing (karyotype, microarray, or targeted genetic testing), 23% received a genetic diagnosis which included sex chromosome abnormalities, non-sex chromosome abnormalities, androgen receptor mutations, and Smith-Lemli-Opitz syndrome [1]. Diagnosis of partial or complete androgen insensitivity is important, given the risk of testicular tumors, effect on fertility, potential need for hormonal replacement, implications for puberty, and risk for family recurrence [1].
References
[1] Swartz JM, Ciarlo R, Denhoff E, et al. Variation in the clinical and genetic evaluation of undervirilized boys with bifid scrotum and hypospadias. J Pediatr Urol. 2017 Jun;13(3):293.e1-293.e6.
[2] Patel BI, Chauhan J, Patel N, et al. Prenatal Difficult Diagnosis of Perineal Abnormalities by 2D-3D US; Turns Out to Be Severe Hypospadias with Bifid scrotum - A Case Report. Med J Obstet Gynecol. 2024 May;12(1):1182.
[3] Yu X, Nassar N, Mastroiacovo P, et al. Hypospadias Prevalence and Trends in International Birth Defect Surveillance Systems, 1980–2010. Eur Urol. 2019 Jul 9;76(4):482–490.
[4] López Soto A, Meseguer González JL, Velasco Martínez M, et al. Sonographic evaluation of fetal scrotum, testes and epididymis. Obstet Gynecol Sci. 2021 Jun 28;64(5):393–406.
[5] Achiron R, Pinhas-Hamiel O, Zalel Y, et al. Development of fetal male gender: prenatal sonographic measurement of the scrotum and evaluation of testicular descent. Ultrasound Obstet Gynecol. 1998 Apr;11(4):242-5.
[6] Pajkrt E, Petersen OB, Chitty LS. Fetal genital anomalies: an aid to diagnosis. Prenat Diagn. 2008 May;28(5):389-98.
[7] Li X, Liu A, Zhang Z, et al. Prenatal diagnosis of hypospadias with 2-dimensional and 3-dimensional ultrasonography. Sci Rep. 2019 Jun 17;9(1):8662.
[8] Meizner I, Mashiach R, Shalev J, et al. The 'tulip sign': a sonographic clue for in-utero diagnosis of severe hypospadias. Ultrasound Obstet Gynecol. 2002 Mar;19(3):250-3.
[9] Köhler B, Schumacher V, l'Allemand D, et al. Germline Wilms tumor suppressor gene (WT1) mutation leading to isolated genital malformation without Wilms tumor or nephropathy. J Pediatr. 2001 Mar;138(3):421-4.
[10] Köhler B, Lin L, Mazen I, et al. The spectrum of phenotypes associated with mutations in steroidogenic factor 1 (SF-1, NR5A1, Ad4BP) includes severe penoscrotal hypospadias in 46,XY males without adrenal insufficiency. Eur J Endocrinol. 2009 Aug;161(2):237–242.
[11] Swartz JM, Ciarlo R, Guo MH, et al. Two unrelated undervirilized 46,XY males with inherited NR5A1 variants identified by whole exome sequencing. Horm Res Paediatr. 2016 Aug 24;87(4):264–270.
[12] Wang Y, Li Q, Xu J, et al. Mutation analysis of five candidate genes in Chinese patients with hypospadias. Eur J Hum Genet. 2004 Sep;12(9):706-12.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Padmanaban Koochu Govindaraju United Kingdom Sonographer

belen garrido Spain Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Mayank Chowdhury India Physician
Ivan Ivanov Russian Federation Physician
CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician

Rushina Patel United States Sonographer

Peter conner Sweden Physician
Marianovella Narcisi Italy Physician

Amparo Gimeno Spain Physician

Elena Andreeva Russian Federation Physician

Basem Hamed United States

Muradiye YILDIRIM Turkey Physician
ALBANA CEREKJA Italy Physician
Eti Zetounie Israel Sonographer

Deval Shah India Physician

Murat Cagan Turkey Physician

Laurie Briare United States Sonographer

Assaad Kesrouani United States Physician

Siddhesh Rajiwade India Maternal fetal medicine specialist
Büşra Cambaztepe Turkey Physician

gholamreza azizi Iran, Islamic Republic of Physician

Ionut Valcea Romania Physician

Hien Nguyen Van Viet Nam Physician

Kathrine Montagne United States Sonographer

Arati Appinabhavi India Physician

CHERYL TURNER United States Sonographer

Sandhy Prayudhana Indonesia Physician

TUAN NGUYEN THE Viet Nam Physician

Rupal Sasani India Physician
philip pattyn Belgium Physician
Eylem Eşsizoğlu Turkey Physician

Wiku Andonotopo Indonesia Physician

Petra Barboríková Slovakia Physician

Nguyễn Lê Hoàng Viet Nam Physician

Denys Saitarly Israel Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician
Elizabeth Smith United States Sonographer

Le Duc Viet Nam Physician
Dr Dhara patel India Physician

Lívia Scatrut Brazil Physician

Hana Habanova Slovakia Physician

Yücel Kaya Turkey Physician

Dr Mayur C Trivedi India Physician

Gnanasekar Periyasamy India Physician
Jagdish Suthar India Physician

Dr Othman Alasali Jordan Physician

LEVENT KANDEMİR Turkey Physician

Luis Iglesias Gutiérrez-Cecchini Spain Physician

Victor Hugo Ribeiro Brazil Physician

Fco Javier Martínez Cortés Spain Physician

Aditya Baldania India Physician