Case of the Week #614
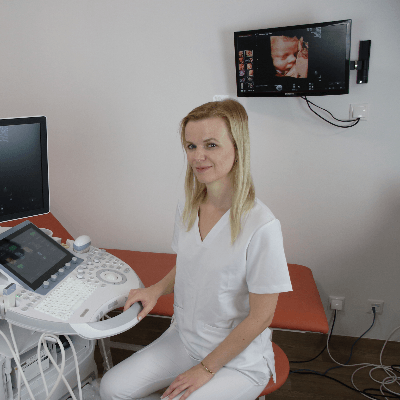
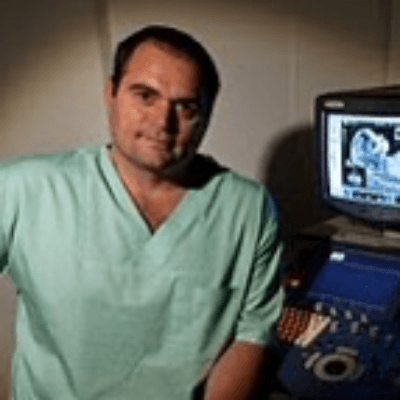
Nemocnica Agel Zvolen, Zvolen, Slovakia
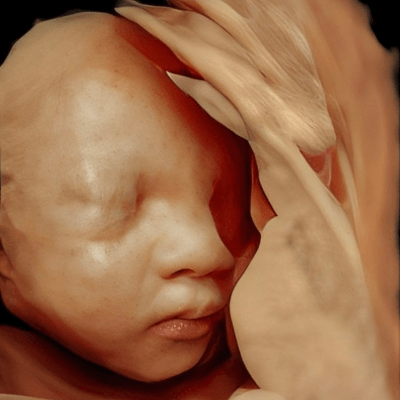
37-year-old G3P0 was examined in our clinic at 20 weeks of pregnancy. Family history was negative and the pregnancy came from nonconsanguineous couple. In the first pregnancy, there was intrauterine fetal death at 19 weeks. Pathological examination showed abnormal placentation and intrauterine growth restriction. The second pregnancy was a spontaneous abortion in the 8th week. Due to her obstetric history, the patient underwent additional hematologic and genetic examination with negative results.


View the Answer Hide the Answer
Answer
We present a case of Hypoplastic left heart syndrome (HSLS). Parents opted for termination of pregnancy.
Our images revealed:
- Video 1: Four chamber view – the left ventricle is smaller in size, not reaching the apex of the heart
- Video 2: Four chamber view
- Video 3: Four chamber view with Doppler mapping – restricted flow across mitral valve and reverse flow across foramen ovale
- Video 4: Three-vessel-trachea view – dilated pulmonary artery and reverse flow in the Aortic arch
- Video 5: Pulmonary artery
- Video 6: Aortic and pulmonary arch – reverse flow across the Aorta
- Video 7: Diameter of the Aorta
- Video 8: Diameter of the pulmonary artery
Discussion
Hypoplastic left heart syndrome is the group of congenital malformations in which there is underdevelopment of the left side of the heart. Hypoplasia of the left ventricle and left ventricular outflow tract is present in every case. The incidence of hypoplastic left heart syndrome is about 2-9% of all congenital heart disease and occurs in 1 in 10,000 live births. We recognize two major types of hypoplastic left heart syndrome: the first type is characterized by mitral and aortic atresia, and the second type has only aortic atresia with a hypoplastic, but patent mitral valve. Hypoplastic left heart syndrome can include other cardiac anomalies characterized by severe hypoplasia of the left ventricle and include aortic coarctation, Shone complex and unbalanced atrioventricular septal defect.
On prenatal ultrasound, the dilated right ventricle is closer to the sternum in the 4-chamber view. The left ventricle can vary in size from invisible, small or dilated. In cases with a dilated left ventricle, the shape of the ventricle is globular with hyperechogenic endocardium (fibroelastosis) and there is the presence of a hypoplastic mitral valve with severe regurgitation. The left heart never reaches the apex of the heart. On color doppler, there is minimal flow across the aortic valve. The flow across the mitral valve can be restricted due to atresia or reversed due to hypoplasia. The aorta is hypoplastic, with no significant or retrograde flow from ductus arteriosus. In the three-vessel view, a dilated pulmonary artery and small aorta are detected. In the three-vessel-trachea view, there is a significant difference in size of the structures, with no or retrogarde flow in the aorta. In utero, a patent foramen ovale is fundamental for the development of the fetus. Due to higher pressures in the left side of the heart, reverse flow (left to right) can be detected. The diagnosis of restrictive foramen ovale can be supported by showing an abnormal pulmonary venous flow with a negative A wave.
In fetuses with hypoplastic left heart syndrome, approximately 15-20% have extracardiac anomalies including congenital diaphragmatic hernia, brain, gastrointestinal, renal and skeletal malformations. Genetic and chromosomal anomalies including Turner syndrome, trisomy 18 and trisomy 13, occur in 15% of fetuses and 3% of neonates, thus karyotyping should be performed.
Prenatal prognostic factors include left ventricle size and function, mitral valve presence and function, size of the aorta and aortic root, the direction of flow across the aortic arch, foramen ovale flow, function of the tricuspid valve and right ventricle, pulmonary venous flow, endocardial fibroelastosis and associated anomalies. If the size of the ascending aorta is greater than 2mm at birth, the Norwood correction can be done. In cases with highly restrictive foramen ovale, the prognosis of the fetus is poor.
Differentiating between critical aortic stenosis and severe coarctation of the aorta can be difficult. It relies on the presence of flow across the mitral and aortic valves and normal contractility of the left ventricle.
During pregnancy, serial ultrasounds are performed every 4 to 6 weeks. Delivery should be planned in a tertiary center as closure of the ductus arteriosus presents a neonatal emergency. Severe atrioventricular valvar restriction is almost always lethal. Treatment with balloon atrial septoplasty in early childhood is possible in children with an intact atrial septum. In utero treatment with balloon valvuloplasty is indicated in fetuses with critical aortic stenosis and dilated left ventricle to prevent the development of hypoplastic left heart syndrome. Surgical treatment for hypoplastic left heart syndrome is heart transplantation or palliative Norwood procedure, which converts the heart to univentricular circulation in three stages. Mortality for hypoplastic left heart syndrome is the highest among congenital heart diseases and untreated can be up to 100%. In a low risk group, the overall survival is 65%-75% while in the high risk group, survival drops to 37%.
References:
[1] Paladini D, et al. "Congenital heart disease“, Ultrasound of congenital fetal anomalies. Boca Raton: CRC Press; 2014, p.189-191
[2] Rychik J, Szwast A, Natarajan S, et al. Perinatal and early surgical outcome for the fetus with hypoplastic left heart syndrome: a 5 year single institutional experience. Ultrasound Obstet Gynecol. 2010 Oct;36(4):465-70.
[3] Wilkins-Haug E, Benson CB, Tworetzky W, et al. In-utero intervention for hypoplastic left heart syndrome — a perinatologist's perspective. Ultrasound Obstet Gynecol. 2005 Oct;26(5):481-6.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician
paola quaresima Italy Physician

Pawel Swietlicki Poland Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician

Gayatri K India Physician

Vladimir Lemaire United States Physician
Shilpen Gondalia India Physician
Ivan Ivanov Russian Federation Physician

Boujemaa Oueslati Tunisia Physician

Tatiana Koipish Belarus Physician

carlos lopez Venezuela Physician

CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician
Anita Silber Israel Physician

Rakhi Agarwal India Physician

Kimberly Delaney United States Sonographer

Olivia Ionescu United Kingdom Physician
Marianovella Narcisi Italy Physician

Javier Ayala Spain Physician

Faten Badr Egypt Physician

Michaela Benešová United States

Selvanandhini Gopalasundaram India Physician
Eti Zetounie Israel Sonographer

Deval Shah India Physician

Murat Cagan Turkey Physician

gholamreza azizi Iran, Islamic Republic of Physician
Gayane Begjanyan Armenia Physician

Ionut Valcea Romania Physician

Yannie Yuen Yee Chan Hong Kong Physician

reyhan ayaz Turkey Physician

Hien Nguyen Van Viet Nam Physician
Jose Sanin Colombia Physician

Kathrine Montagne United States Sonographer

Miguel Sanchez Mexico Physician

Almaz Kinzyabulatov Russian Federation Physician

Kareem Haloub Australia Physician
Zuzana Briešková Slovakia Physician

András Weidner Hungary Physician
Fred Pop Uganda Sonographer

Annette Reuss Germany Physician

Vandana Yakub India Physician
shruti Agarwal India Physician
Jay Vaishnav India Physician
CHERYL TURNER United States Sonographer

Ismail Guzelmansur Turkey Physician

Shelby Duncan United States Sonographer

Sruthi Pydi India Physician

Laura Wharton United Kingdom Physician

Deniz Delibaş Turkey Physician

Jacqueline L J Cullen United States Sonographer

Rupal Sasani India Physician
Hiral Shah India Fetal Medicine specialist

Petra Barboríková Slovakia Physician

Recep Taha Agaoglu Turkey Physician

Dennis Wood United States Sonographer

Nguyễn Lê Hoàng Viet Nam Physician

Denys Saitarly Israel Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician

Costin Radu Lucian Romania Physician

Joel Dery United Kingdom Sonographer

Hetal Patel India Physician
Le Duc Viet Nam Physician

PADMA Priya DHARSHINI India Physician

Hana Habanova Slovakia Physician

Tamara Yarygina Russian Federation Physician
Marius Bogdan Muresan Romania Physician
Gnanasekar Periyasamy India Physician

Văn Kiệt Võ Viet Nam Physician

Meera Trivedi India Physician
Navya Sri Mopada India Physician
Jagdish Suthar India Physician

Alesia Haidalenak Belarus Physician
Petra Tallova Slovakia Physician

Severina Gesheva United States Sonographer

Camila Cabrera United States Physician

Sami Melinkovich United States Sonographer
CARLOS JOSE PIÑA VILLEGAS Peru MEDICO MATERNO FETAL

Ayisha Shaikh United Kingdom Physician

Clary Gomerez United States Sonographer

Ruby Lin United States Physician

Erika Sembrera Peru Physician

Raoul Desbriere France Physician

vivian camposano Australia Sonographer