Case of the Week #613
(1) Centre d Echographie et de Medecine Foetale; Belveder Centre, Tunis, TUNISIE; (2) Hospital Recoletas Campo Grande, Valladolid, Spain












View the Answer Hide the Answer
Answer
We present a case of Beckwith-Wiedemann syndrome. The child was born at term by cesarean section with a birth weight of 4800g and underwent operation for his omphalocele. Genetic testing of chromosome 11p15 demonstrated hypomethylation at the TSS-DMR region of the KCNQ1OT1 gene. At follow up 4 years later, the child is doing well without significant problems.
Our images demonstrate:
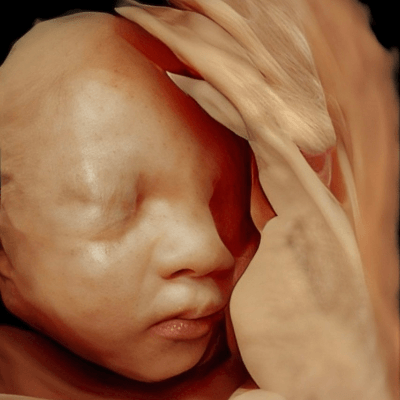
- Image 1: Omphalocele contains only the intestines; normal bladder, absence of macroglossia, male gender
- Image 2 and 3: anomaly of the posterior fossa with communication of V4 with the greater cistern. There is an appearance of elevation of the cerebellar tentorium and unclear morphology of the vermis that may be explained by the elevation of the vermis and early gestational age (18 weeks)
- Video 1: abdominal and thoracic scan demonstrated absence of other anomalies. In particular, absence of cardiac anomalies and cardiomegaly
- Image 4: at 23 weeks gestation, the kidneys are normal and the renal pelvises are not particularly dilated
- Image 5: a small cyst in the spleen
- Image 6: at 23 weeks, there is still absence of macroglossia
- Image 7: absence of anomalies of the posterior fossa with normal cerebellar tent, vermis and absence of signs suggestive of Dandy Walker syndrome
- Image 8: normal face without macroglossia
- Image 9: normal ear and hand without polydactyly
- Image 10: at 30 weeks, there is mild pyelectasis
- image 11: at 30 weeks, there is slight nephromegaly
- Image 12: at 30 weeks, slight macrosomia probably underestimated by the "usual" method of measuring abdominal girth that excludes the omphalocele

Discussion
Beckwith–Wiedemann syndrome (OMIM 130650), a phenotypically and genetically heterogeneous disorder, is the most common congenital disorder characterized by neonatal overgrowth and gigantism [1]. Also known as Wiedemann-Beckwith syndrome and Beckwith-Wiedemann spectrum, the condition is characterized by a variable set of anomalies that most commonly include macrosomia, macroglossia, visceromegaly, and omphalocele [2]. It was first described in 1963 by John Bruce Beckwith, an American pediatric pathologist [3], and in 1964 by Hans-Rudolf Wiedemann, a German paediatrician geneticist [4]. It was originally called EMG syndrome based on the presence of Exomphalos, Macroglossia, and Gigantism in many cases [5]. Prenatal diagnosis of Beckwith–Wiedemann syndrome was first reported in 1980 by Weinstein and Anderson [6] and, since then, about 60 cases have been reported in the literature.
Its prevalence is approximately 1 in 10,000 live births [7], though it is 10 times greater (1 in 1000) in children conceived through assisted reproductive techniques [8] and in monozygotic twins, in particular female twins with asymmetric expression of the syndrome [9]. The genetic mechanisms leading to Beckwith–Wiedemann syndrome are complex, and involve alterations in the balance of growth regulatory genes located at chromosome 11p15.5 [10-13]. This region includes two differentially methylated regions, known as IC1 and IC2, that control imprinting within the domain. Epigenetics and genomic defects are observed in 70% to 80% of patients, though 20% are idiopathic. Mutations identified are loss of methylation of IC2 on the maternal chromosome (50%), paternal uniparental disomy of 11p15.5 (20%), gain of methylation of IC1 on the maternal chromosome (5%), mutation of the maternal CDKN1C allele (5% of sporadic cases, but up to 40% in familial cases), and cytogenetic duplications, inversions or translocations of 11p15.5 (1%). Some correlation between genotype and phenotype has been identified, with abdominal wall defects dominant in fetuses with IC2 hypomethylation while macrosomia, organomegaly and tumoral predisposition are more frequent in patients with IC1 hypermethylation [12]. Genetic testing for Beckwith–Wiedemann syndrome can include DNA methylation studies, single-gene testing, copy number analysis for 11p15.5, chromosomal microarray, karyotype, and use of multigene panels that include genes in the Beckwith–Wiedemann syndrome critical region [13].
Beckwith-Wiedemann syndrome is considered a clinical spectrum, in which affected individuals may have many or only some of the characteristic clinical features [14]. Postnatally, these include overgrowth, macroglossia, abdominal wall defects, renal and urologic malformations, neonatal hyperinsulinemic hypoglycemia, lateralized overgrowth, lobe creases or helical pits, facial nevus flammeus, organomegaly, and increased risk of embryonal tumors in childhood [13,14]. The risk is increased (4%-21%) for embryonal tumors, particularly Wilms tumor (nephroblastoma) but also hepatoblastoma, neuroblastoma, adrenocortical carcinoma, and rhabdomyosarcoma [15].
Prenatal diagnosis of Beckwith–Wiedemann syndrome is challenging because although the omphalocele, the most common prenatal finding, is usually detected early in pregnancy, associated findings of macrosomia, macroglossia, and visceromegaly, when present, are detected later in gestation [16]. Some prenatal signs should alert the clinician, such as the rapid increase in growth of the abdominal circumference in the 3rd trimester with associated polyhydramnios, especially in the absence of maternal diabetes. Ultrasound examination should then look for signs more suggestive of Beckwith-Wiedemann syndrome, such as macroglossia, visceromegaly and placental hypertrophy [17]. Abdominal wall defects (umbilical hernia or omphalocele) are the most prevalent prenatal sign detected in 43% of cases, which is followed by polyhydramnios (33%), macrosomia (33%), macroglossia (18%), organomegaly including nephromegaly, hepatomegaly, and cardiomegaly (18%), placentomegaly (8%), tumors (4%), and anomalies of the corpus callosum (1%) [12]. In addition to abnormalities of the corpus callosum, Gardiner et al [18] reported seven cases of Beckwith-Wiedemann syndrome associated with posterior fossa abnormalities including Blake’s pouch cyst, hypoplasia of the inferior part of the vermis, and Dandy–Walker malformation. These cases nearly all had molecular defects in the imprinted domain 2. Several systems classifying prenatal findings into major and minor criteria have been described, however the results are limited due to the large number and variability of the findings in Beckwith–Wiedemann syndrome and the difficulty in identifying these prenatally [19, 20].
Placental enlargement and/or thickening is sometimes accompanied by characteristic ultrasound findings (edematous and spongy placenta with multiple small lacunae, without high vascularisation) that correspond to the pathologic diagnosis of placental mesenchymal dysplasia [21]. Placentomegaly may cause an increase in beta-hCG and inhibin-A levels, while high levels of maternal serum alpha fetoprotein and uE3 may be associated with visceral organ enlargement including liver and adrenal gland. Given that elevation of all biomarkers of the triple screen/quad test is rarely reported to be specific to any other disorder, this finding may be clinically useful for early detection of Beckwith-Wiedemann syndrome [21, 22].
Some maternal pregnancy complications have a higher frequency in Beckwith-Wiedemann syndrome, especially gestational hypertension, pre-eclampsia, HELLP syndrome and eclampsia. Placentomegaly may contribute to excessive beta-hCG levels seen in the second trimester. The relationship between increased beta-hCG and AFP levels, and preeclampsia is well established. Additionally, elevated beta-hCG can contribute to overstimulation of the ovaries [22]. Premature labor and delivery can occur in pregnancies affected with Beckwith-Wiedemann syndrome due to preeclampsia, macrosomia and polyhydramnios. Delivery should occur in a tertiary center to prevent complications from macroglossia and hypoglycemia, and if present, perform surgical repair of the omphalocele. After childhood, complications are infrequent, and development is usually normal unless there are hypoxic episodes or untreated hypoglycemia [2, 23].
Several overgrowth syndromes that show features of macrosomia but are usually not associated with visceromegaly, macroglossia, or omphalocele should be differentiated from Beckwith-Wiedemann syndrome, such as Simpson–Golabi–Behmel syndrome, Perlman syndrome, and Sotos syndrome [12].
References
[1] Vora N, Bianchi DW. Genetic considerations in the prenatal diagnosis of overgrowth syndromes. Prenat Diagn. 2009 Oct;29(10):923-9.
[2] Gallerneau F. Beckwith-Wiedemann Syndrome. In: Copel JA, ed. Obstetric Imaging. Fetal diagnosis and care, 2nd ed. Elsevier, Philadelphia, PA, 2018; pages 462-466.e1.
[3] Beckwith JB. Extreme cytomegaly of the adrenal fetal cortex, omphalocele, hyperplasia of the kidneys and pancreas, and Leydig cell hyperplasia—another syndrome? Presented at the Annual Meeting of Western Society for Pediatric Research, Los Angeles, November 11, 1963.
[4] Wiedemann HR. Complexe malformatif familial avec hernie ombilicale et macroglossie—un “syndrome nouveau”?. J Genet Hum. 1964 Sep;13:223-32.
[5] Irving IM. The "E.M.G." syndrome (Exomphalos, Macroglossia, Gigantism). Prog Pediatr Surg. 1970;1:1-61.
[6] Weinstein L, Anderson C. In utero diagnosis of Beckwith--Wiedemann syndrome by ultrasound. Radiology. 1980 Feb;134(2):474.
[7] Mussa A, Russo S, De Crescenzo A, et al. Prevalence of Beckwith-Wiedemann syndrome in North West of Italy. Am J Med Genet A. 2013 Oct;161A(10):2481-6.
[8] Mussa A, Molinatto C, Cerrato F, et al. Assisted Reproductive Techniques and Risk of Beckwith-Wiedemann Syndrome. Pediatrics. 2017 Jul;140(1):e20164311.
[9] Franceschini P, Guala A, Vardeu MP, et al. Monozygotic twinning and Wiedemann-Beckwith syndrome. Am J Med Genet. 1993 May 15;46(3):353-4.
[10] Tenorio J, Romanelli V, Martin-Trujillo A, et al. Clinical and molecular analyses of Beckwith-Wiedemann syndrome: Comparison between spontaneous conception and assisted reproduction techniques. Am J Med Genet A. 2016 Oct;170(10):2740-9.
[11] Traisrisilp K, Chankhunaphas W, Sirilert S, et al. New genetic and clinical evidence associated with fetal Beckwith-Wiedemann syndrome. Prenat Diagn. 2021 Jun;41(7):823-827.
[12] Ma GC, Chen TH, Wu WJ, et al. Proposal for Practical Approach in Prenatal Diagnosis of Beckwith-Wiedemann Syndrome and Review of the Literature. Diagnostics (Basel). 2022 Jul 13;12(7):1709.
[13] Shuman C, Kalish JM, Weksberg R. Beckwith-Wiedemann Syndrome. 2000 Mar 3 [Updated 2023 Sep 21]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024.
[14] Brioude F, Kalish JM, Mussa A, et al. Expert consensus document: Clinical and molecular diagnosis, screening and management of Beckwith-Wiedemann syndrome: an international consensus statement. Nat Rev Endocrinol. 2018 Apr;14(4):229-249.
[15] Rump P, Zeegers MP, van Essen AJ. Tumor risk in Beckwith-Wiedemann syndrome: A review and meta-analysis. Am J Med Genet A. 2005 Jul 1;136(1):95-104.
[16] Shieh HF, Estroff JA, Barnewolt CE, et al. Prenatal imaging throughout gestation in Beckwith-Wiedemann syndrome. Prenat Diagn. 2019 Aug;39(9):792-795.
[17] Le Vaillant C, Beneteau C, Chan-Leconte N, et al. Le syndrome de Beckwith-Wiedemann: que faut-il rechercher en anténatal? À propos d'une série de 14 cas [Beckwith-Wiedemann syndrome: What do you search in prenatal diagnosis? About 14 cases]. Gynecol Obstet Fertil. 2015 Nov;43(11):705-11.
[18] Gardiner K, Chitayat D, Choufani S, et al. Brain abnormalities in patients with Beckwith-Wiedemann syndrome. Am J Med Genet A. 2012 Jun;158A(6):1388-94.
[19] Williams DH, Gauthier DW, Maizels M. Prenatal diagnosis of Beckwith-Wiedemann syndrome. Prenat Diagn. 2005 Oct;25(10):879-84.
[20] Carli D, Bertola C, Cardaropoli S, et al. Prenatal features in Beckwith-Wiedemann syndrome and indications for prenatal testing. J Med Genet. 2021 Dec;58(12):842-849.
[21] Jatavan P, Tongsong T, Traisrisilp K. Fetal Beckwith-Wiedemann syndrome associated with abnormal quad test, placental mesenchymal dysplasia and HELLP syndrome. BMJ Case Rep. 2021 Jun 24;14(6):e243415.
[22] Aagaard-Tillery KM, Buchbinder A, Boente MP, et al. Beckwith-Wiedemann syndrome presenting with an elevated triple screen in the second trimester of pregnancy. Fetal Diagn Ther. 2007;22(1):18-22.
[23] Kagan KO, Berg C, Dufke A, et al. Novel fetal and maternal sonographic findings in confirmed cases of Beckwith-Wiedemann syndrome. Prenat Diagn. 2015 Apr;35(4):394-9.
Discussion Board
Winners

Guest United States

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Dmitry Abelov Russian Federation Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician

RITIKA BHANDARI India Physician
Ivan Ivanov Russian Federation Physician

Tatiana Koipish Belarus Physician

Aysegul Ozel Turkey Physician

Alvaro Gómez Mexico Physician

Gayane Besedina Russian Federation Physician

Olivia Ionescu United Kingdom Physician

Annette Reuss Germany Physician

Muradiye YILDIRIM Turkey Physician
Eti Zetounie Israel Sonographer

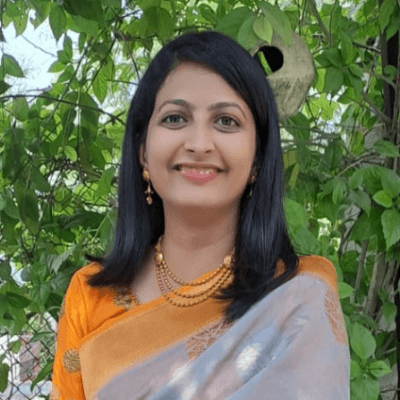
Deval Shah India Physician
SAMUEL GELVEZ TELLEZ Colombia Physician

Murat Cagan Turkey Physician

Sonio Sonio France AI

Ionut Valcea Romania Physician

Yannie Yuen Yee Chan Hong Kong Physician

Halil Korkut Dağlar United States Physician

Seda Cam Turkey Physician

Almaz Kinzyabulatov Russian Federation Physician

Ismail Guzelmansur Turkey Physician

Sruthi Pydi India Physician

Laura Wharton United Kingdom Physician

Deniz Delibaş Turkey Physician

Ashraf Elkashef Egypt Physician
philip pattyn Belgium Physician

Petra Barboríková Slovakia Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician
Le Duc Viet Nam Physician
Dr Dhara patel India Physician
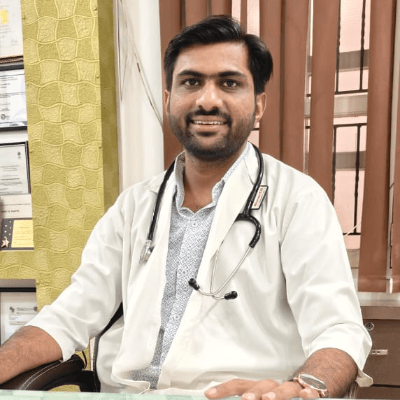
Jagdish Suthar India Physician

Rachel Escobedo United States Sonographer