Case of the Week #607
(1) Femicare, Center of prenatal ultrasonographic diagnostics, Martin, Slovakia; (2) RDMS RDCS-FE Maternal Fetal Associates in Reston, Virginia
A 27-year-old primigravida with no significant medical history presented to our office at 20 weeks, 4 days of her pregnancy. Following findings were observed.





View the Answer Hide the Answer
Answer
We present a case of Osteogenesis Imperfecta Type III (progressive deforming osteogenesis imperfecta).
Our examination revealed following findings:
- Image 1, Video 1: Small chin, mild micrognathia
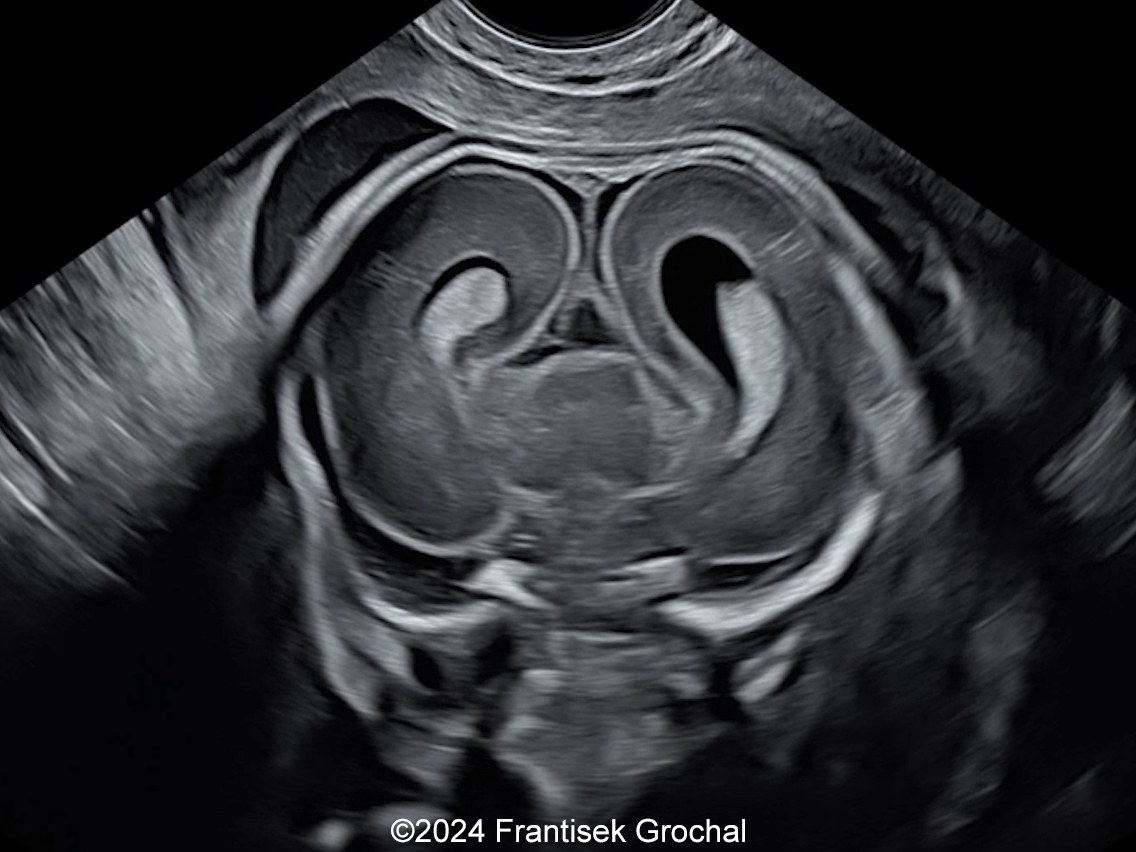
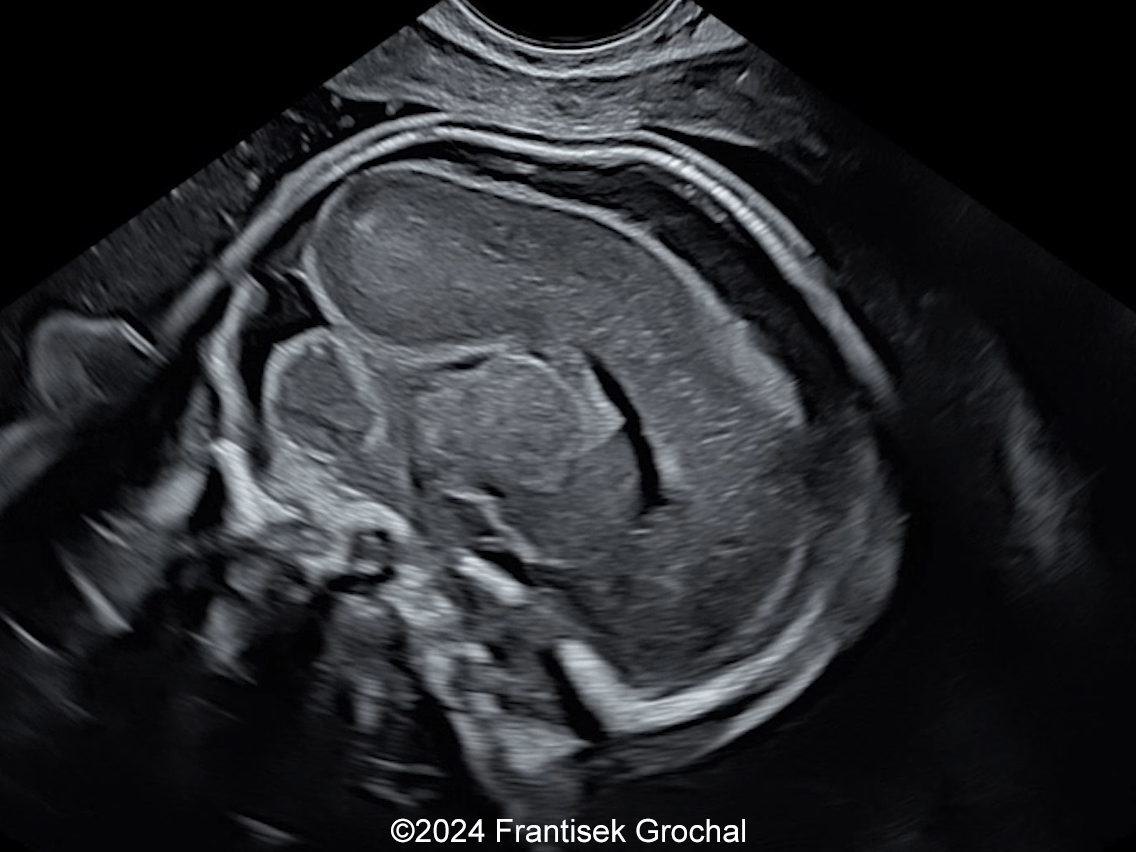
- Image 2-3, Video 2: Easy-compressible skull bones
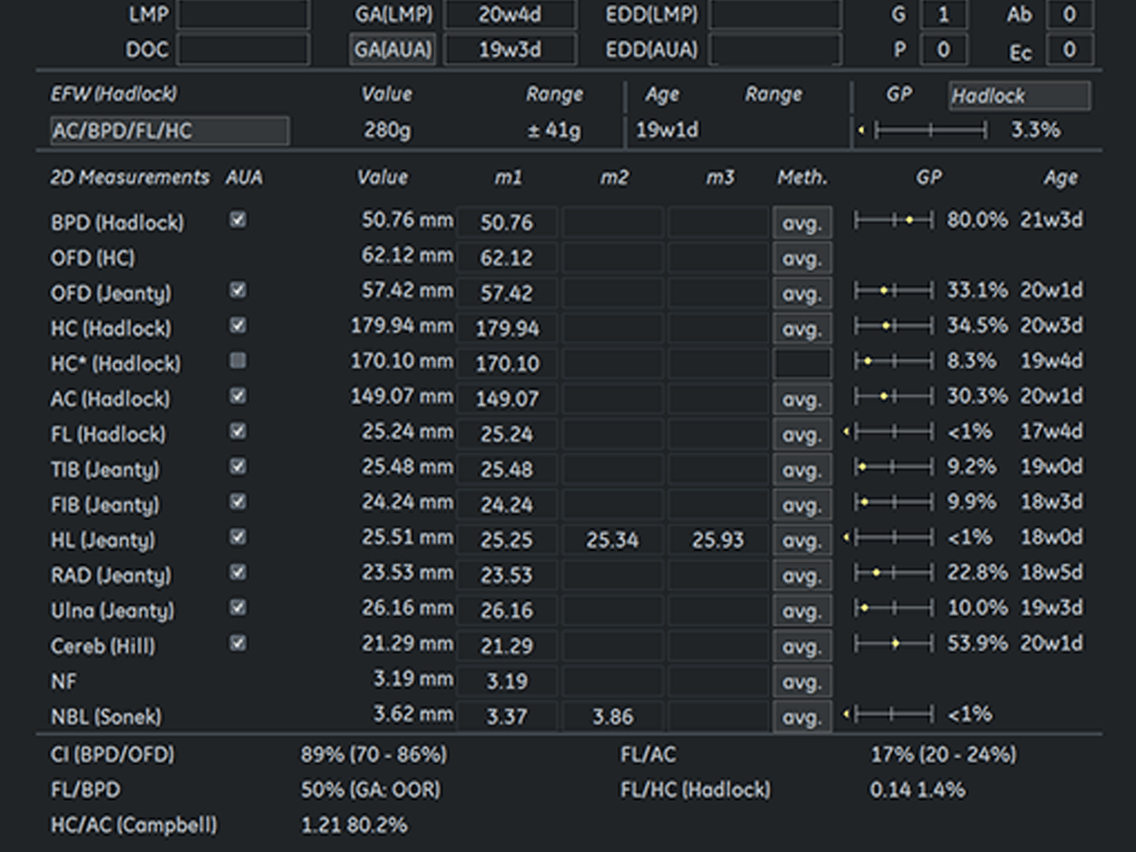
- Image 4 : Biometry demonstrated mild brachycephalic macrocrania and short long bones (femur, humus, tibia, ulna)
- Image 5, Video 3: Bowed femurs and tibia
- Image 6, Video 4: Normal scapulae and spine, no rib fractures seen
- Image 7-8: Small chin and wide anterior fontanelle
Non-lethal osteogenesis imperfecta was presumed and the patient underwent amniocentesis confirming the diagnosis. The parents opted for termination of the pregnancy.
Discussion
Osteogenesis imperfecta is a genetic disorder characterized by impaired collagen synthesis, which causes bones to be fragile and more prone to fractures. This condition manifests in various subtypes, affecting approximately 1 in 20,000 births. Each subtype of osteogenesis imperfecta leads to varying degrees of short-limbed dwarfism. The bone fragility associated with osteogenesis imperfecta can result in perinatal mortality or severe lasting deformities that persist throughout a person's life.
Osteogenesis imperfecta is often inherited in an autosomal dominant manner, though may be sporadic. Mutations in COL1A1 and COL1A2, which encode the α1 and α2 chains of type I collagen, either cause a structural or quantitative deficiency of type I collagen. Type II is perinatally lethal, while Type III is the most severe form observed in patients who survive the neonatal period. Starting from birth, individuals with Type III osteogenesis imperfecta often suffer from multiple fractures and deformities affecting the long bones, skull, and spine, such as kyphoscoliosis, severe dwarfism due to compression fractures of the spine, bowed legs, and disruptions in growth plate function. Additionally, they may experience respiratory difficulties that can be life-threatening, cardiac valve regurgitation, hearing loss in adulthood, brittle teeth, and blueish discoloration of the sclera.
Prenatal ultrasonography proves indispensable for the early and accurate diagnosis of osteogenesis imperfecta by identifying key indicators such as fractures, calvarial characteristics, and femoral abnormalities. Differentiating between the lethal type II and severe type III osteogenesis imperfecta remains complex; however, the triad of extreme femoral shortening, multiple fractures in a single bone, and calvarial demineralization has been associated with lethality. Early in gestation, absence of posterior acoustic shadowing can indicate lethal osteogenesis imperfecta. Additional factors associated with lethal skeletal dysplasia include severe pulmonary hypoplasia, a femur length-to-abdominal circumference (FL-to-AC) ratio of less than 0.16, and polyhydramnios. Our case demonstrated bowed long bones but no fractures, and a compressible skull, though the demineralization was not so severe to demonstrate absence of posterior acoustic shadowing. We therefore felt this case was most consistent with nonlethal osteogenesis imperfecta.
Differential diagnoses include thanatophoric dysplasia and achondrogenesis which both present with extremely short limbs, small chest, and macrocrania, though fetuses with thanatophoric dysplasia have normal bone mineralization without fractures and those with achondrogenesis can have decreased mineralization with occasional fractures. The integration of advanced prenatal imaging techniques is critical for deepening our understanding of osteogenesis imperfecta and facilitating informed clinical management.
While in the past, caesarean delivery was thought to be safer for the delivery of neonates with osteogenesis imperfecta, recent studies have shown that the rate of fractures was not significantly different between those delivered by caesarean section and those delivered vaginally.
References
Deguchi M, Tsuji S, Katsura D, et al. Current Overview of Osteogenesis Imperfecta. Medicina (Kaunas). 2021 May; 57(5): 464.
Discussion Board
Winners

Boujemaa Oueslati Tunisia Physician

Jesus Cortez Venezuela Physician