Case of the Week #591
(1) Ridham Hospital, Anand, Gujarat, India; (2) Centro Médico Recoletas, Valladolid, Spain
A 22-year-old G2P1 woman with no pertinent medical history came for first trimester screening with following findings:


View the Answer Hide the Answer
Answer
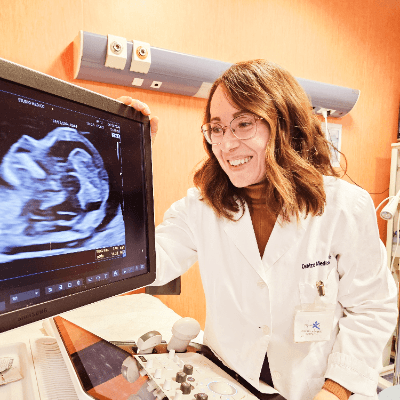
We present a case of first-trimester cord entanglement in monochorionic, monoamniotic twins. The patient opted to terminate the pregnancy despite being offered intensive monitoring.
Our images revealed the following findings:
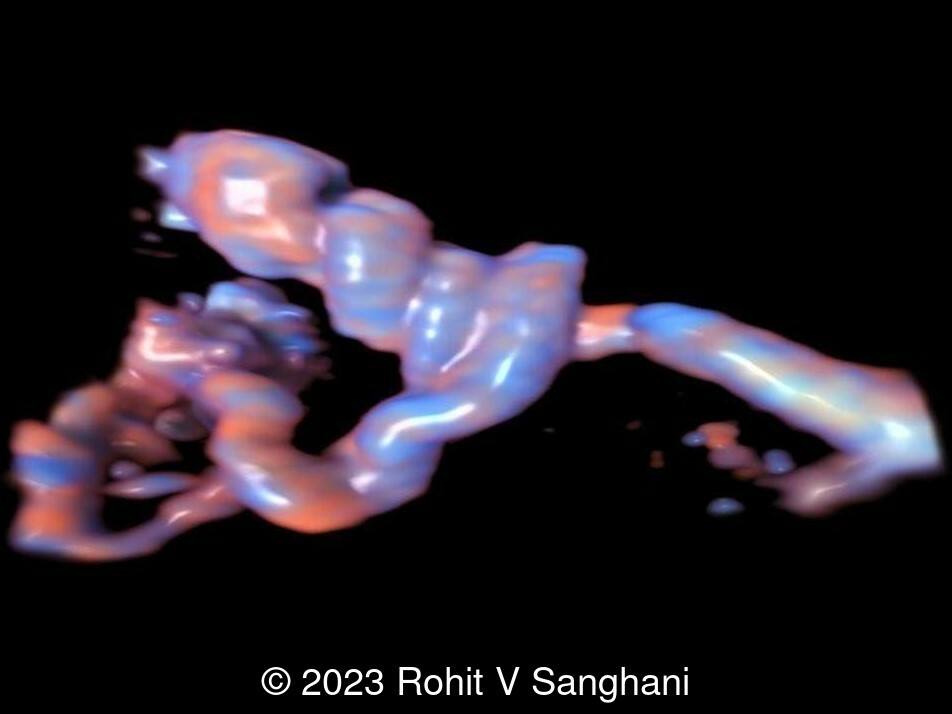
- Image 1, Video 1, 2 : Monochorionic monoamniotic twin showing entanglement of umbilical cords
- Image 2 : 3D rendered image demonstrating monochorionic, monoamniotic twins with no intertwin membrane
Discussion
Monochorionic monoamniotic twin pregnancy is characterized by the presence of two fetuses sharing a single placenta and a single amniotic cavity. Its prevalence at birth is 0.8 to 1 per 10,000 pregnancies [1], approximately 1% of all twin pregnancies and 5% of all monochorionic twins [2-4]. Monoamniotic twins are the result of the late splitting of a single embryo between day 8 and day 13 after fertilization and are more common after in vitro fecundation/embryo transfer [5].
The presence of both fetuses in the same amniotic sac may predispose to cord entanglement which can result in compression of one or both cords, and fetal death. In addition, these pregnancies are subject to the risks of monochorionic twin pregnancy, which include twin-twin transfusion syndrome, twin anemiae polycythemia sequence, selective intrauterine growth restriction and twin reversed arterial perfusion sequence, as well as to the general risks of twin pregnancy such as preterm birth, increased congenital anomalies, and increased perinatal mortality [4].
Cord entanglement is pathognomonic for monoamniotic twins. It can be seen as early as 12 -13 weeks as intertwined umbilical cords showing different fetal heart rates. Cord entanglement is thought to be caused by normal fetal movement. It probably occurs early in pregnancy when the ratio of amniotic cavity to fetal size is largest, and fetal movements relative to each other are greatest. Cord entanglement is considered a key factor for increased risk of miscarriage, fetal malformations, intrauterine or neonatal death, and high perinatal mortality rates which are estimated between 15 and 30% [1, 6, 7]. Cord entanglement can appear in up to 74% of all monochorionic monoamniotic pregnancies [8]. Although cord entanglement is a specific pathology of monochorionic monoamniotic pregnancies, it can also occur in monochorionic diamniotic pregnancies after rupture of the dividing membrane [9].
Diagnostic ultrasonographic criteria currently adopted by most authors for making an accurate antenatal diagnosis of monochorionic-monoamniotic twin pregnancy include same-sex twins, a single placenta, no dividing membrane, normal amniotic fluid volume, unrestricted fetal movement, and cord entanglement [10, 11]. When the resolution of ultrasound was not as high as at present, the finding of entangled umbilical cords demonstrated the absence of a membrane separating the fetuses making it possible to diagnose a twin pregnancy as monochorionic monoamniotic [12].
On ultrasound examination two umbilical cords are seen to originate from a single placenta, occasionally at short distance from each other. Several loops of apparently intertwined umbilical cord may represent either the entangled cords of two twins, or the redundant cord of a single twin folded upon itself. It is essential to follow both cords from separate placental insertions, and from each fetal umbilicus to the entanglement [13]. Color and pulsed Doppler velocimetry play an important role in the demonstration of cord entanglement as it develops [14, 15]. The visualization of two distinct arterial waveform patterns of different heart rates within the same pulsed wave sampling gate (“galloping pattern”) is indicative of monoamnioticity and of cord entanglement in the first trimester [15]. In addition, pulsed Doppler is essential in the clinical management of this pathology. Abnormal pulsed Doppler sonographic findings range in severity from the presence of a diastolic notch, which is not indicative of an adverse perinatal outcome, to absent or reversed diastolic velocity in the umbilical artery and even pulsatile flow in the umbilical vein, possibly carrying a worse prognosis [16-19]. Prenatal mortality is also conditioned by the location of the cord entanglement, being higher in cases closer to the fetus than to the placenta [20]. Three-dimensional ultrasound (color Dopler and surface-rendered image) has been suggested as a new method for demonstrating cord entanglement [21, 22].
Perinatal outcome in monoamniotic twins has improved in recent years due to intensive fetal surveillance, which includes multiple ultrasound scans and fetal heart rate monitoring, performed either outpatient or inpatient. Balancing the risk of prematurity at various gestational ages and the risk of intrauterine death after that gestational age, most studies advocate delivery at 32 to 33 weeks with preference for caesarean section over vaginal delivery [3, 23].
References:
[1] Glinianaia SV, Rankin J, Khalil A, et al. Prevalence, antenatal management and perinatal outcome of monochorionic monoamniotic twin pregnancy: a collaborative multicenter study in England, 2000-2013. Ultrasound Obstet Gynecol. 2019 Feb;53(2):184-192.
[2] Benirschke K. The placenta in twin gestation. Clin Obstet Gynecol. 1990 Mar;33(1):18-31.
[3] Gilad N, Pruthi V, Shinar S, et al. Monochorionic Monoamniotic Twin Pregnancy. In: Khalil A, Lewi L, and Lopriore E, ed. Twin and Higher-order Pregnancies. Springer Nature Switzerland AG 2021; pages 275-285.
[4] Shub A, Walker SP. Planned early delivery versus expectant management for monoamniotic twins. Cochrane Database Syst Rev. 2015 Apr 23;2015(4):CD008820.
[5] Alikani M, Cekleniak NA, Walters E, et al. Monozygotic twinning following assisted conception: an analysis of 81 consecutive cases. Hum Reprod. 2003 Sep;18(9):1937-43.
[6] Madsen C, Søgaard K, Zingenberg H, et al. Outcomes of monoamniotic twin pregnancies managed primarily in outpatient care-a Danish multicenter study. Acta Obstet Gynecol Scand. 2019 Apr;98(4):479-486.
[7] Périnet AC, Massoud M, Picard L, et al. Comparison of foetal and neonatal mortality of monochorionic monoamniotic and monochorionic biamniotic twin pregnancies [Article in French]. Gynecol Obstet Fertil Senol. 2023 Feb;51(2):123-128.
[8] Dias T, Mahsud-Dornan S, Bhide A, et al. Cord entanglement and perinatal outcome in monoamniotic twin pregnancies. Ultrasound Obstet Gynecol. 2010 Feb;35(2):201-4.
[9] Ito A, Nakata M, Oji A, et al. Diagnosis of umbilical cord entanglement in a monochorionic diamniotic twin pregnancy with spontaneous septostomy of the dividing membranes using dual-gate Doppler imaging. J Med Ultrason (2001). 2018 Jan;45(1):189-192.
[10] Shveiky D, Ezra Y, Schenker JG, et al. Monoamniotic twins: an update on antenatal diagnosis and treatment. J Matern Fetal Neonatal Med. 2004 Sep;16(3):180-6.
[11] Deutsch AB, Miller E, Spellacy WN, et al. Ultrasound to identify cord knotting in monoamniotic monochorionic twins. Twin Res Hum Genet. 2007 Feb;10(1):216-8.
[12] Nyberg DA, Filly RA, Golbus MS, et al. Entangled umbilical cords: a sign of monoamniotic twins. J Ultrasound Med. 1984 Jan;3(1):29-32.
[13] Townsend RR, Filly RA. Sonography of nonconjoined monoamniotic twin pregnancies. J Ultrasound Med. 1988 Dec;7(12):665-70.
[14] Belfort MA, Moise KJ Jr, Kirshon B, et al. The use of color flow Doppler ultrasonography to diagnose umbilical cord entanglement in monoamniotic twin gestations. Am J Obstet Gynecol. 1993 Feb;168(2):601-4.
[15] Overton TG, Denbow ML, Duncan KR, et al. First-trimester cord entanglement in monoamniotic twins. Ultrasound Obstet Gynecol. 1999 Feb;13(2):140-2.
[16] Abuhamad AZ, Mari G, Copel JA, et al. Umbilical artery flow velocity waveforms in monoamniotic twins with cord entanglement. Obstet Gynecol. 1995 Oct;86(4 Pt 2):674-7.
[17] Rosemond RL, Hinds NE. Persistent abnormal umbilical cord Doppler velocimetry in a monoamniotic twin with cord entanglement. J Ultrasound Med. 1998 May;17(5):337-8.
[18] Suzuki S, Ishikawa G, Sawa R, et al. Umbilical venous pulsation indicating tight cord entanglement in monoamniotic twin pregnancy. J Ultrasound Med. 1999 Jun;18(6):425-7.
[19] Aurioles-Garibay A, Hernandez-Andrade E, Romero R, et al. Presence of an umbilical artery notch in monochorionic/monoamniotic twins. Fetal Diagn Ther. 2014;36(4):305-11.
[20] Arabin B, Hack K. Is the location of cord entanglement associated with antepartum death in monoamniotic twins? Ultrasound Obstet Gynecol. 2009 Feb;33(2):246-7.
[21] Kuwata T, Matsubara S, Suzuki M. 3D color Doppler of monoamniotic twin cord entanglement. Arch Gynecol Obstet. 2010 May;281(5):973-4.
[22] Hanaoka U, Tenkumo C, Ito M, et al. Three-dimensional surface-rendered imaging of cord entanglement in monoamniotic twins. Arch Gynecol Obstet. 2012 Oct;286(4):1091-2.
[23] Van Mieghem T, De Heus R, Lewi L, et al. Prenatal management of monoamniotic twin pregnancies. Obstet Gynecol. 2014 Sep;124(3):498-506.
Discussion Board
Winners

Emad Abdelrahim Elshorbagy Egypt Physician

Igor Yarchuk United States Sonographer

Ana Ferrero Spain Physician

Mayank Chowdhury India Physician

Vladimir Lemaire United States Physician

Ivan Ivanov Russian Federation Physician

Boujemaa Oueslati Tunisia Physician

Tatiana Koipish Belarus Physician
carlos lopez Venezuela Physician

Aysegul Ozel Turkey Physician
Halil Mesut Turkey Physician

Rushina Patel United States Sonographer

Alvaro Gómez Mexico Physician
RANJAN DUTTA India Physician

lan nguyen xuan Viet Nam Physician
Kimberly Delaney United States Sonographer
Marianovella Narcisi Italy Physician

Faten Badr Egypt Physician
Shari Morgan United States Sonographer

Amparo Gimeno Spain Physician

ALBANA CEREKJA Italy Physician

Yana Semina Russian Federation Physician

Irina Kuchma United States Sonographer

Eti Zetounie Israel Sonographer

Murat Cagan Turkey Physician
Eslam Adel ammar Egypt Physician

Charlotte Conturie United States Physician

Loai Said Palestinian Territory, Occupied Physician

Büşra Cambaztepe Turkey Physician
Rasha Abo Almagd Egypt Physician

Ionut Valcea Romania Physician
Cong Bang Duong Viet Nam Physician

Đặng Mai Quỳnh Viet Nam Physician

Hien Nguyen Van Viet Nam Physician

Borisova Elena Russian Federation Physician

Miguel Sanchez Mexico Physician

Almaz Kinzyabulatov Russian Federation Physician

Kareem Haloub Australia Physician
Zuzana Briešková Slovakia Physician

Martina Vagaská Slovakia Physician

Subapriya Kandasamy India Physician

Anette Beverdam Netherlands Sonographer

mohamed ateya Egypt Physician
shay kevorkian Israel Physician

SAVITA SHIRODKAR India Physician

Mahmoud Moussa United Kingdom Physician

Mariam Tezhaeva United Kingdom Physician

Hiral Shah India Fetal Medicine specialist

SHILPA KISHORE India Physician

Dr. Suguna Sunil India Fetal Medicine Specialist

Emily Witt United States Sonographer

Alicja Mankiewicz Poland Physician

Heidi Winkels United States Sonographer

Ellen Cates United States Sonographer

Nestor Ferrer Venezuela Physician