Case of the Week #583
(1) High Risk Pregnancy Center, Hera Women's Health (Las Vegas and Reno, Nevada USA); (2) Centro Médico Recoletas. Valladolid. Spain
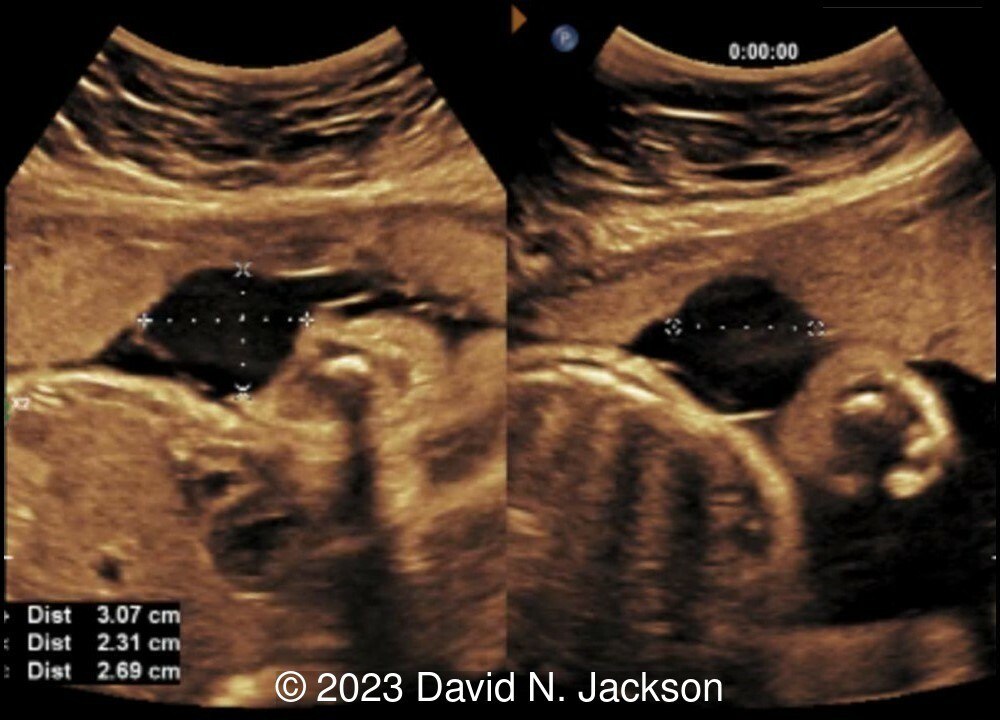
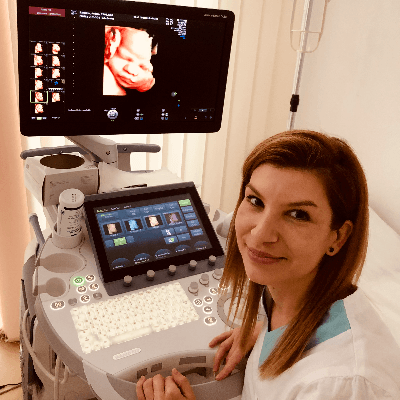
27-year-old gravida 1 was admitted at 31 3/7 weeks due to the following findings at the placental cord insertion.
View the Answer Hide the Answer
Answer
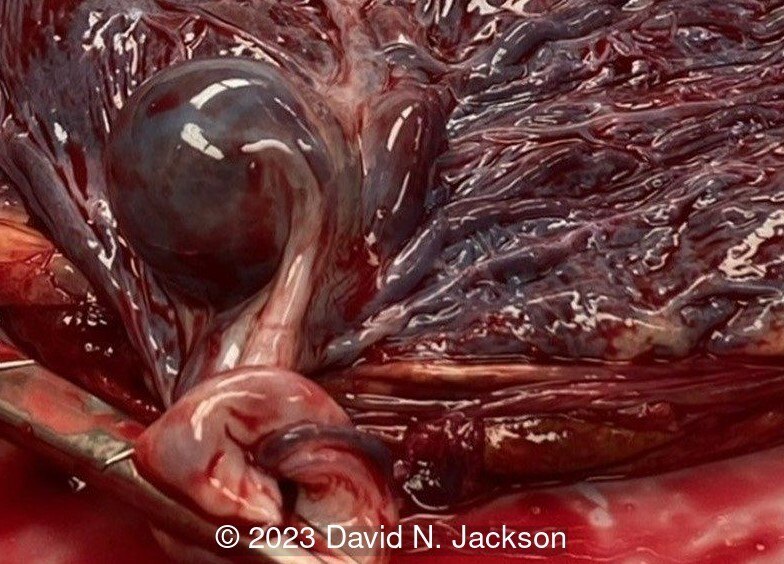
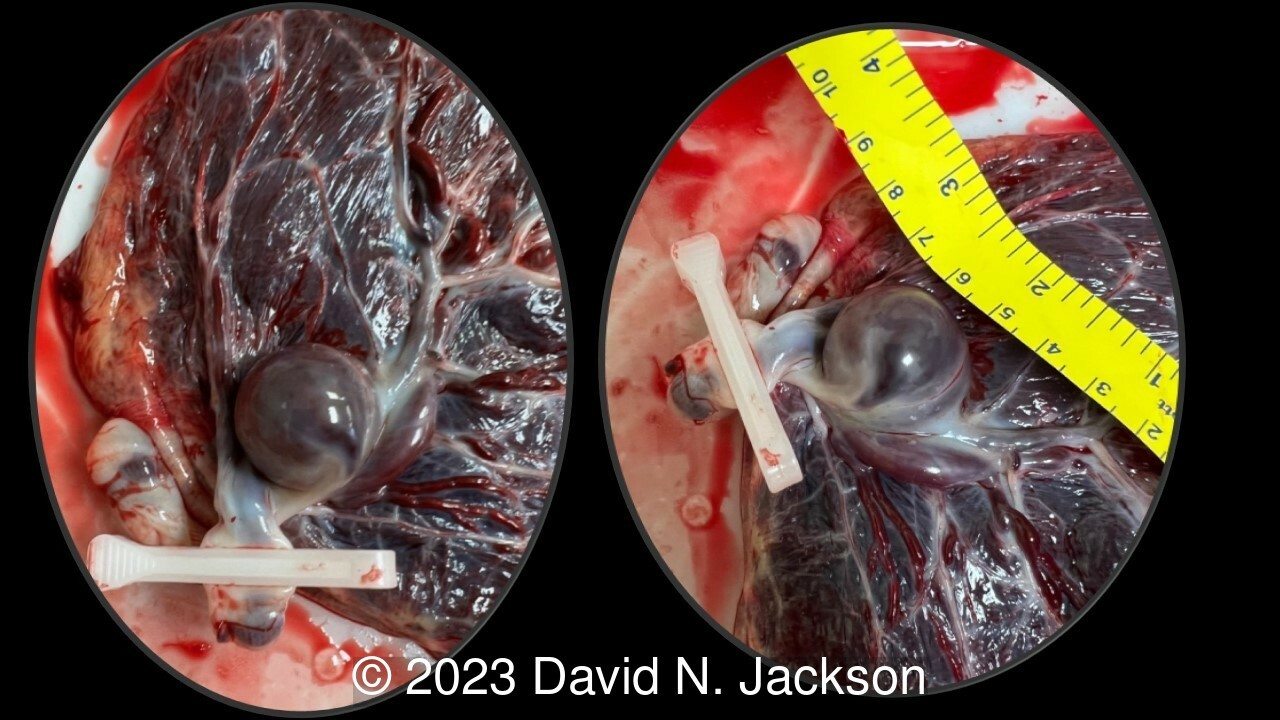
We present a case of umbilical artery aneurysm.
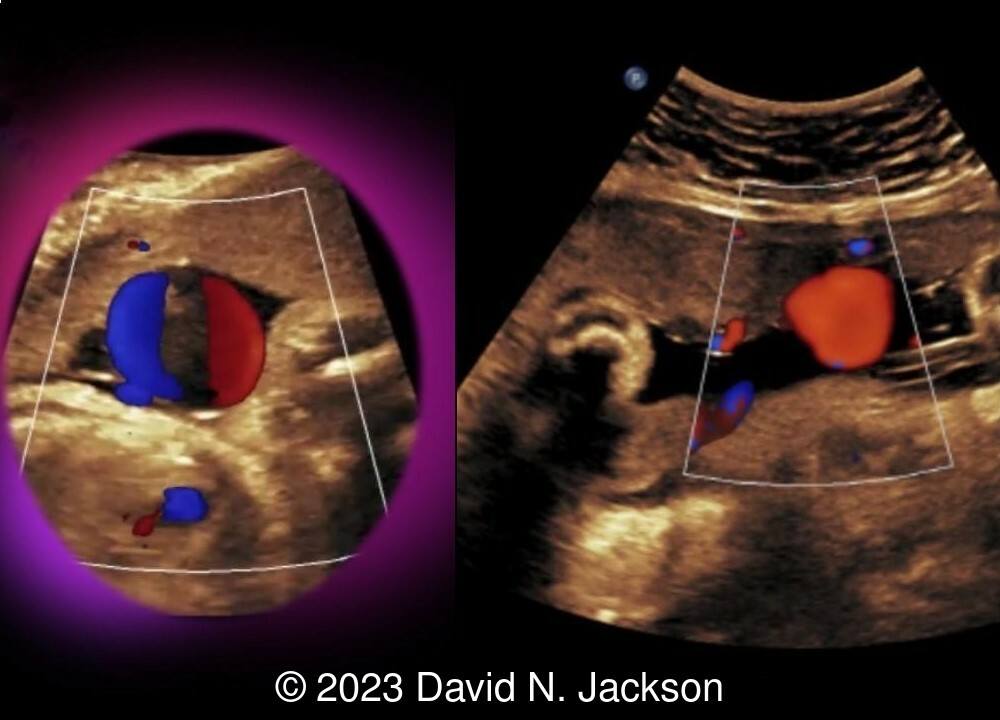
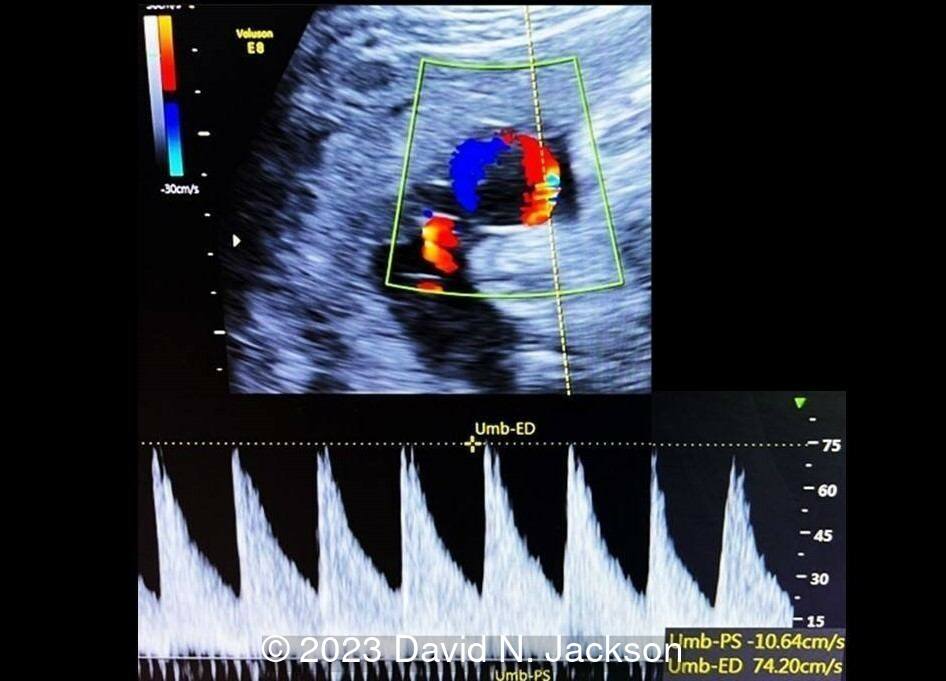
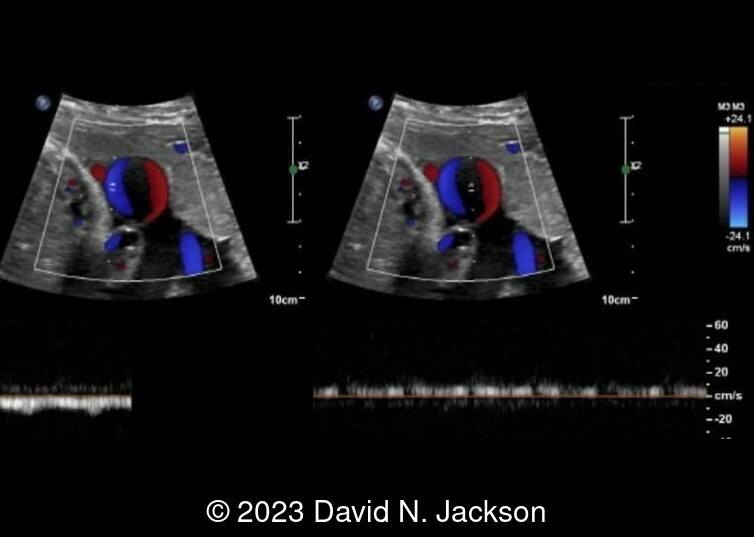
Ultrasound demonstrates a 3 cm pulsatile echolucency at the cord insertion. Interestingly, the Doppler flow showed arterial pulsations on one side, which reduced to venous pulsations on the opposite side of the 3 cm cyst. Concern over thrombosis in the setting of an umbilical artery aneurysm led to the admission of the patient with fetal monitoring 2 hours on and 4 hours off throughout the day. Daily umbilical artery Doppler at the aneurysmal dilation showed an increased peak systolic resistance to 75cm/sec when the fetus pressed against the dilation. When the fetus was not in contact with the aneurysm, the peak systolic velocity of the umbilical artery was 35 cm/s. There was no evidence of mitral regurgitation, cardiomegaly, cardiac failure, or fetal anemia. There was no ascites or evidence of hydrops.
The fetal monitoring did not show decelerations. The daily biophysical profile was reassuring. The patient received betamethasone and magnesium sulfate for fetal neuro protection. After detailed shared decision making, the family opted for delivery at 32 weeks to avoid the possibility of cord thrombosis or emergent delivery with the fetus pressing against the cord. A viable, healthy neonate was delivered without complication by cesarean section.

Discussion
Despite the little importance given to the study of the umbilical cord, there are a considerable number of anomalies that can occur, some with severe consequences. Among them are excessively long or short cords, hyper or hypocoiling of the cord, cysts, single umbilical artery, supernumerary vessels, stricture, velamentous insertion, umbilical vein varix, umbilical artery aneurysm, umbilical vein and arterial thromboses, hematomas, and tumors which can include hemangioma, angiomyxoma, and teratoma [1]. Aneurysms of the umbilical vessels are the least common vascular anomaly of the cord [2].
Dilations of both the vein (varicose vein) and the umbilical arteries (aneurysm) have been described, and present as focal dilatations of the corresponding vessel with vascular flow. The spectral Doppler shows the characteristics of the flow, continuous in the vein and pulsatile in the arteries. Vascular thromboses are more frequent in the dilated umbilical vein than in the artery, and are identifiable on ultrasound as an echogenic zone inside the vessel with turbulent, nonpulsatile flow in the areas of dilation [3].
Prenatal sonographic diagnosis of umbilical artery aneurysms has been reported infrequently and consists of a focal enlargement or dilatation of the umbilical cord. Color and spectral Doppler imaging will confirm the pulsatile arterial nature of blood flow. The finding of a solid area of heterogeneous echogenicity absent of vascularity within the aneurysm represents a mural thrombus. Umbilical artery aneurysms are usually detected in areas near the placental insertion site, and usually during the second or third trimester of gestation [4].
Some authors have reported normal fetal outcomes [4, 5], but an adverse result is more common. Umbilical artery aneurysm has been associated with single umbilical artery [5-7, 9-12], Trisomy 18 [7, 8], cardiac abnormalities [9], fetal growth-restriction [10], and intrauterine fetal death [10-12]. According to the literature, 67% of cases are associated with a single umbilical artery [13]. When a cord possesses only one artery and one vein, the artery undergoes a compensatory increase in diameter. Thinning of the arterial wall in this situation may contribute to aneurysm formation as fetal cardiac output increases with gestational age [6, 7]. Loss of the protective Wharton’s jelly near the placental cord insertion is another possible causative factor [7]. Thrombosis and compression of adjacent vessels have been suggested as potential causes of fetal demise in reported cases of umbilical artery aneurysm [11, 12].
Following diagnosis, detailed sonographic assessment for additional anomalies (including fetal echocardiography), karyotype analysis (non-invasive prenatal testing or amniocentesis), close fetal surveillance for interval growth, fetal well-being, and possible early delivery should be considered [13]. Most authors perform an elective caesarean section to avoid rupture of the aneurysm, but it is not clear if this mode of delivery improves fetal outcomes [9, 13].
The differential diagnosis includes other cystic anomalies of the umbilical cord (true cysts and pseudocysts). If an anechoic cyst is detected in the umbilical cord, Doppler study plays a critical role in differentiating vascular from non-vascular lesions [10].
References
[1] Sherer DM, Al-Haddad S, Cheng R, et al. Current Perspectives of Prenatal Sonography of Umbilical Cord Morphology. Int J Womens Health. 2021 Oct 18;13:939-971. doi: 10.2147/IJWH.S278747.
[2] Kaplan CG. Anatomy and Pathology of the Umbilical Cord. In: Baergen RN, Burton GJ, Kaplan CG, ed. Benirschke's Pathology of the Human Placenta, 7th ed. Springer Nature Switzerland AG, 2022; pages 345-402.
[3] Sánchez-Trujillo L, García-Montero C, Fraile-Martinez O, et al. Considering the Effects and Maternofoetal Implications of Vascular Disorders and the Umbilical Cord. Medicina (Kaunas). 2022 Nov 29;58(12):1754. doi: 10.3390/medicina58121754.
[4] Olog A, Thomas JT, Petersen S, et al. Large umbilical artery aneurysm with a live healthy baby delivered at 31 weeks. Fetal Diagn Ther. 2011;29(4):331-3. doi: 10.1159/000322960.
[5] Vyas NM, Manjeera L, Rai S, et al. Prenatal Diagnosis of Umbilical Artery Aneurysm with Good Fetal Outcome and Review of Literature. J Clin Diagn Res. 2016 Jan;10(1):QD01-3. doi: 10.7860/JCDR/2016/14800.7030.
[6] Hill AJ, Strong TH Jr, Elliott JP, et al. Umbilical artery aneurysm. Obstet Gynecol. 2010 Aug;116 Suppl 2:559-562. doi: 10.1097/AOG.0b013e3181e7d280.
[7] Sepulveda W, Corral E, Kottmann C, et al. Umbilical artery aneurysm: prenatal identification in three fetuses with trisomy 18. Ultrasound Obstet Gynecol. 2003 Mar;21(3):292-6. doi: 10.1002/uog.69.
[8] Berg C, Geipel A, Germer U, et al. Prenatal diagnosis of umbilical cord aneurysm in a fetus with trisomy 18. Ultrasound Obstet Gynecol. 2001 Jan;17(1):79-81. doi: 10.1046/j.1469-0705.2001.00313.x.
[9] Matsuki R, Nakago S, Kato H, et al. Management strategy of umbilical artery aneurysm complicated by cardiac anomaly: case study and literature review. J Matern Fetal Neonatal Med. 2017 Aug;30(15):1809-1812. doi: 10.1080/14767058.2016.1226796.
[10] Sentilhes L, Vivet-Lefébure A, Patrier S, et al. Umbilical artery aneurysm in a severe growth-restricted fetus with normal karyotype. Prenat Diagn. 2007 Nov;27(11):1059-61. doi: 10.1002/pd.1817.
[11] Weber MA, Sau A, Maxwell DJ, et al. Third trimester intrauterine fetal death caused by arterial aneurysm of the umbilical cord. Pediatr Dev Pathol. 2007 Jul-Aug;10(4):305-8. doi: 10.2350/06-07-0136.1.
[12] Shen O, Reinus C, Baranov A, et al. Prenatal diagnosis of umbilical artery aneurysm: a potentially lethal anomaly. J Ultrasound Med. 2007 Feb;26(2):251-3. doi: 10.7863/jum.2007.26.2.251.
[13] Doehrman P, Derksen BJ, Perlow JH, et al. Umbilical artery aneurysm: a case report, literature review, and management recommendations. Obstet Gynecol Surv. 2014 Mar;69(3):159-63. doi: 10.1097/OGX.0000000000000051.
Discussion Board
Winners

Guest United States

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Umber Agarwal United Kingdom Maternal Fetal Medicine

Dmitry Abelov Russian Federation Physician

Larysa Gazarova United States Physician

Andrii Averianov Ukraine Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician

Tatiana Koipish Belarus Physician

Sara Abdallah Salem Egypt Physician
CHARLES SARGOUNAME India Physician

Michal Michna Slovakia Physician
Halil Mesut Turkey Physician

Crismaru Iulia Romania Physician

Suat İnce Turkey Physician
Shari Morgan United States Sonographer

santosh shahare United States Physician

Muradiye YILDIRIM Turkey Physician
Eslam Adel ammar Egypt Physician
Mária Brešťanská Slovakia Physician

Ionut Valcea Romania Physician

aastha mehra India Physician
Martina Vagaská Slovakia Physician
shruti Agarwal India Physician

mohamed ateya Egypt Physician
Qi Tang China Physician

Lynn Davis United States Sonographer

Andrea Stoop-Berends Netherlands Sonographer

Ismail Guzelmansur Turkey Physician

Mariam Tezhaeva United Kingdom Physician

Anitha Christina. M India Physician