Case of the Week #579
High Risk Pregnancy Center, Hera Women's Health (Las Vegas and Reno, Nevada USA)
Case report: A 35-year-old multiparous patient was referred for a consultative ultrasound. Serial ultrasounds were performed between 23 and 38 weeks gestation. The following images were obtained.












View the Answer Hide the Answer
Answer
We present a case of Umbilical Cord Hemangioma
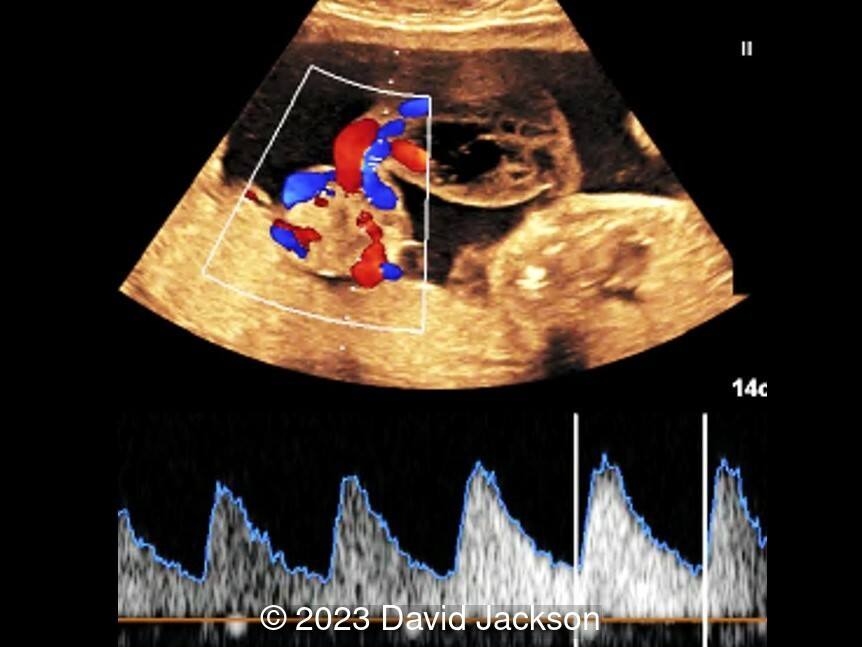
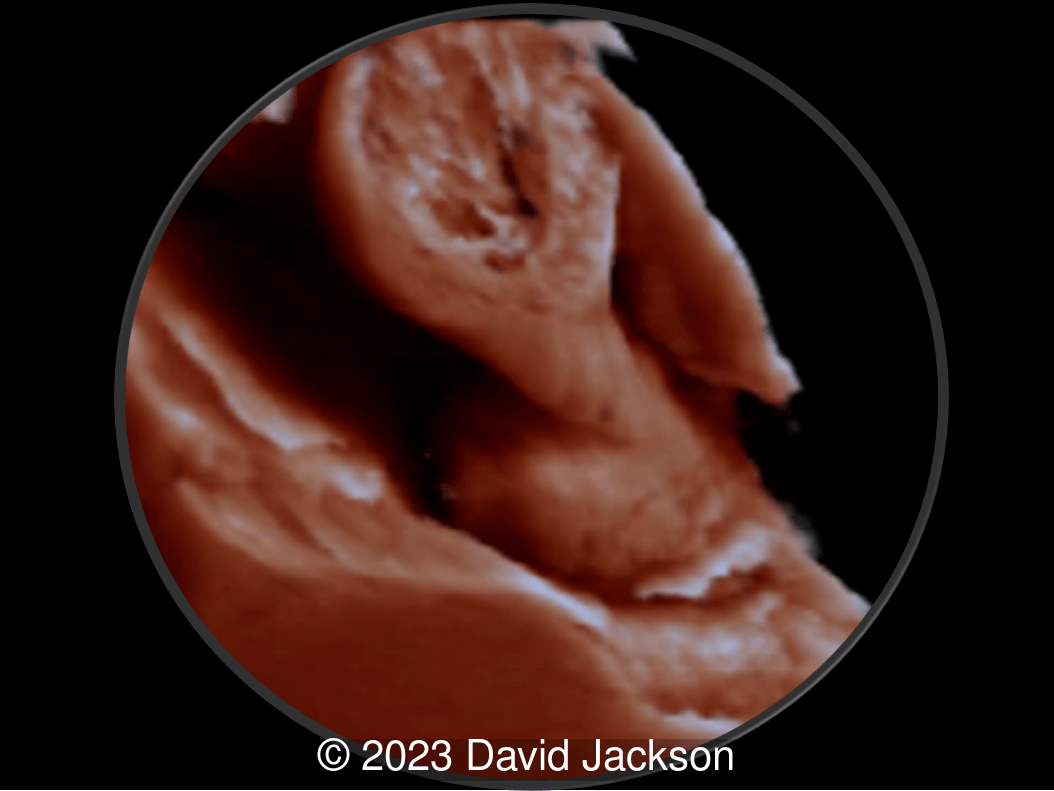
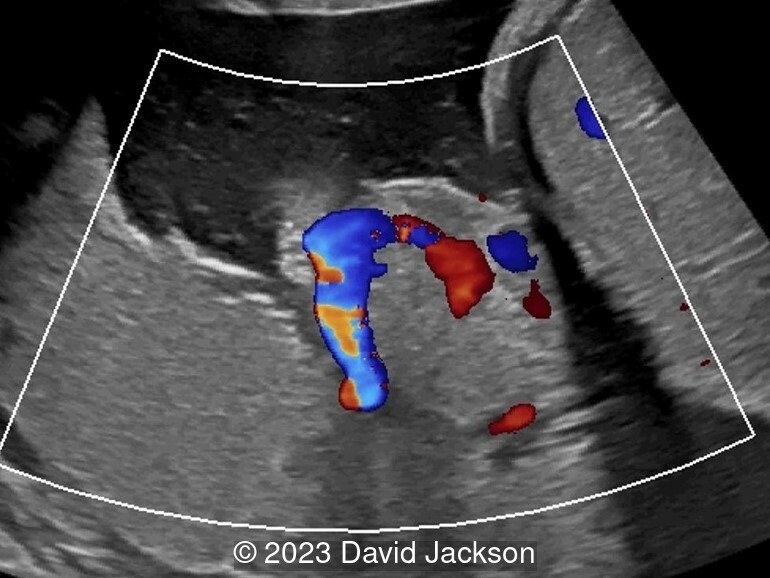
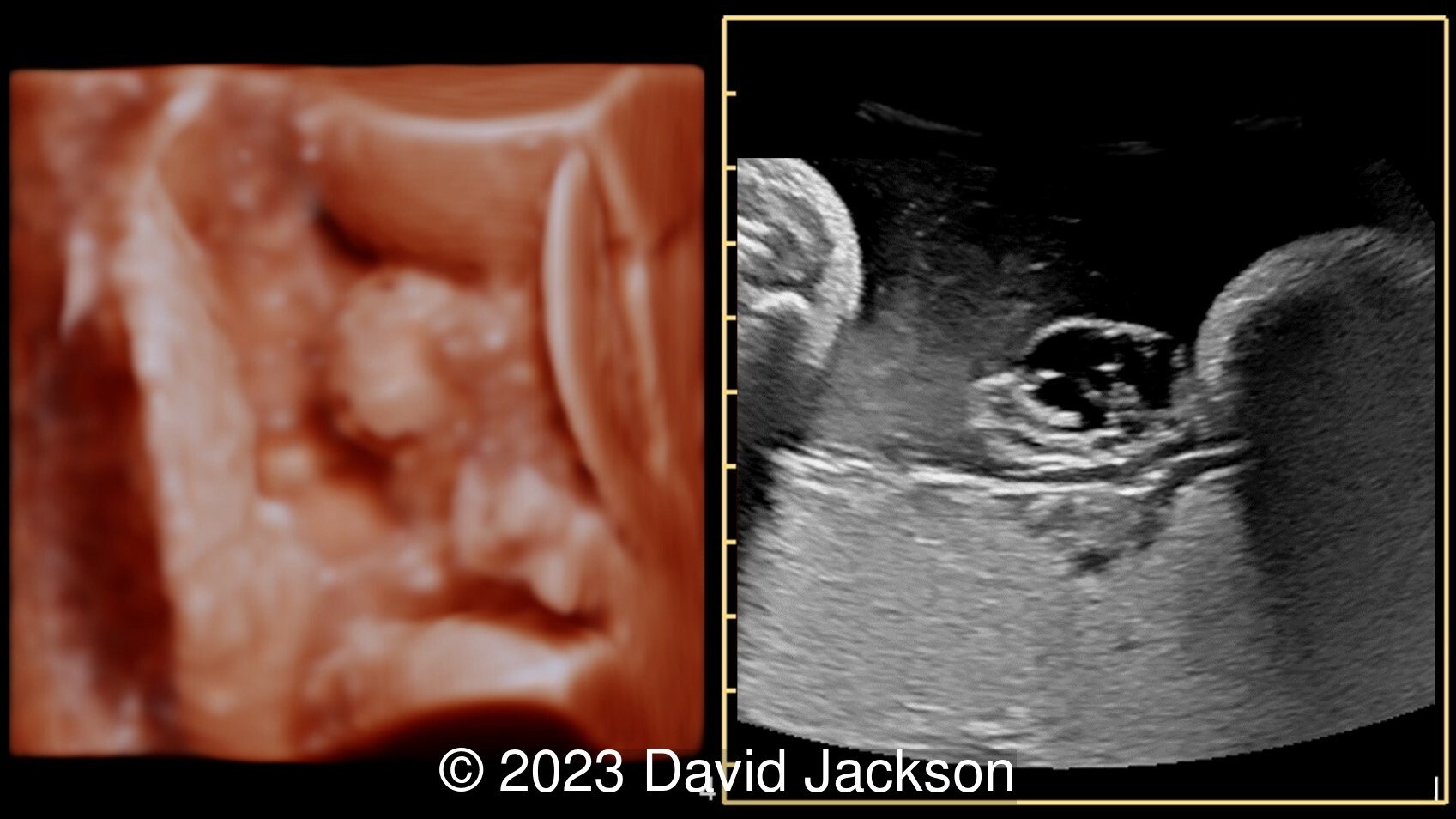
Ultrasound identified an echogenic mass at the umbilical cord insertion, extending up the cord toward the fetus measuring 7.6cm x 7.1cm x 4cm in diameter. Three-dimensional imaging confirmed a central solid tissue nodule and multiple pseudocysts. Doppler indices were without increased resistance. A small umbilical varix was seen. Serial weekly imaging (with biophysical profile and Doppler of the umbilical artery) identified a progressive mass expansion and polyhydramnios development. At 31 weeks, the fetus developed moderate cardiomegaly, mild pericardial effusion, and an altered E/A ratio. At that point, the mass diameter was 12.9cm x 9.6cm x 5cm. Monitoring was increased to twice a week. The mass and cardiac findings stabilized. There were no abnormalities on monitoring or Doppler. She was delivered vaginally at 38 weeks. Mother and baby did well. The child did not require any surgical interventions.
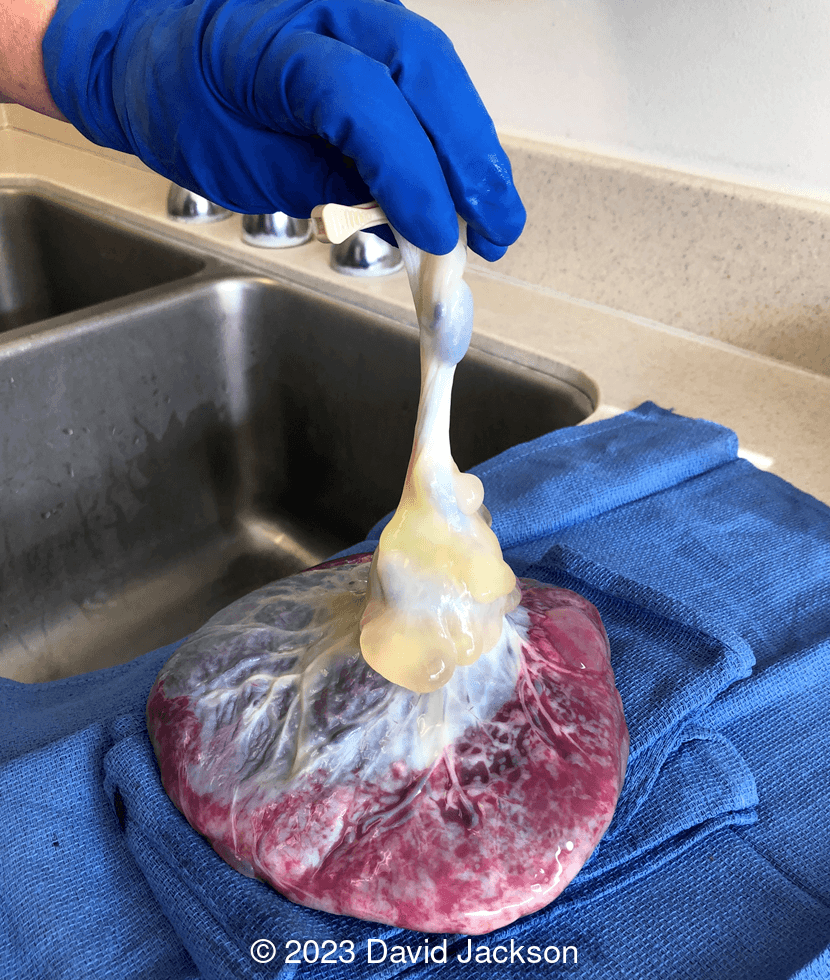
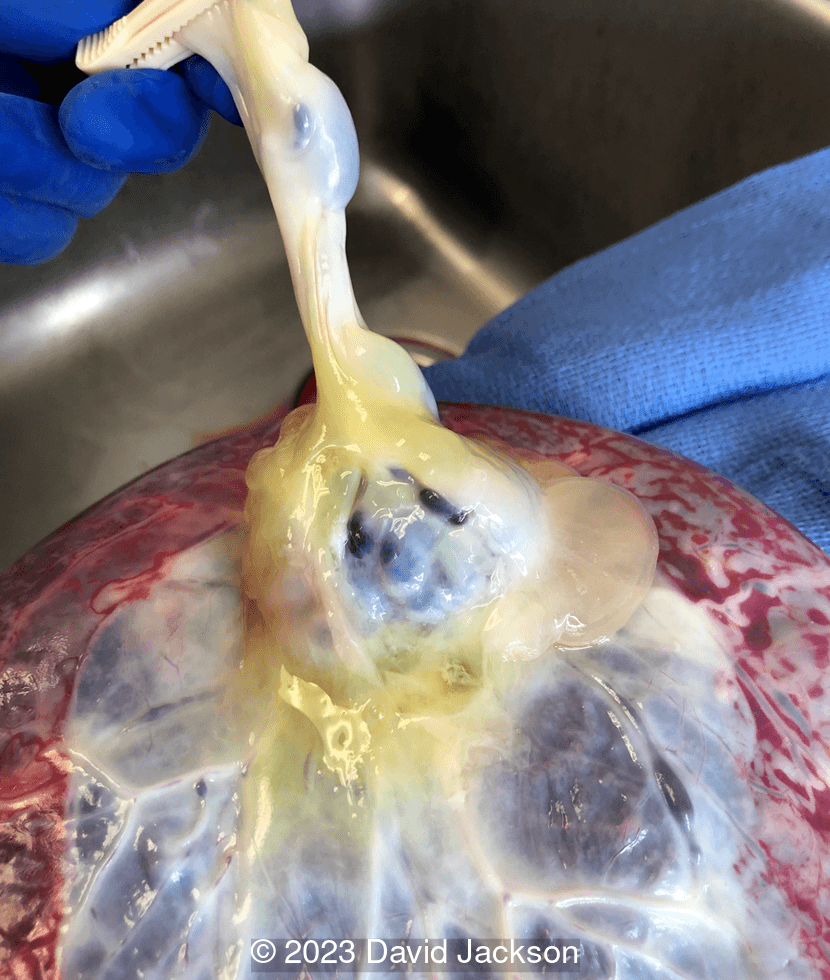
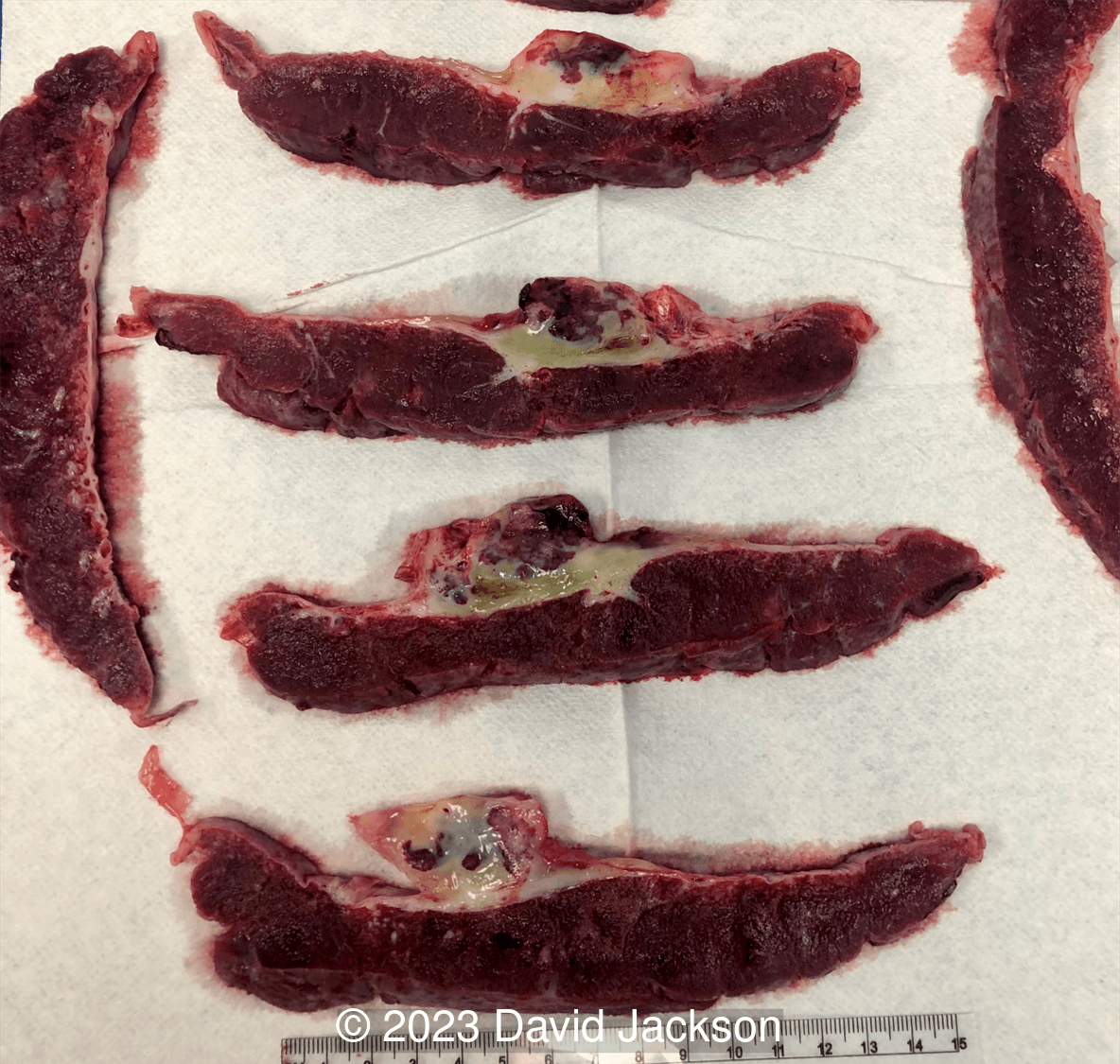
On pathologic examination, the placenta weighed 1187g with a 15.0 x 10.0 x 5.0cm tumor near the umbilical cord insertion at the placenta. The gross pathologic evaluation revealed a dense mass with rubber-like consistency and pseudocyst formation. Histologically there were thin-walled, dilated vascular channels distributed in a myxoid matrix, characteristic of a true hemangioma of the umbilical cord.
Discussion
Umbilical cord hemangiomas are rare tumors of the umbilical cord that require serial evaluation and monitoring when detected on prenatal ultrasound. Since 1951, 56 cases of umbilical cord hemangiomas have been reported in the literature. While most cases result in a live birth, evidence suggests that at least a quarter end in demise and approximately 20% in preterm birth. Reports vary regarding the incidence of maternal complications, growth of the mass, integrity of cord and placental vasculature, amniotic fluid indices, as well as the presence of fetal cardiac dysfunction and other associated anomalies.
While hemangiomas of the placenta are well known, identified in an estimated 1% of pregnancies [1], hemangiomas arising within the umbilical cord are far less common, with only 40 cases published since 1990, 33 of which were identified prenatally. These vascular neoplasms typically originate from the umbilical artery. Histologically, they are characterized by endothelial proliferation and present with a distinct pattern of capillaries embedded within myxoid stroma [2,3]. On examination, the lesion presents as a fusiform swelling comprised of vascularized nodules and pseudocysts that cause expansion of Wharton’s jelly manifesting as cord edema [2,4,5]. Progressive cord edema and pseudocyst degeneration may cause mechanical compression of cord vessels, compromising fetal circulation, and leading to associated complications which include fetal cardiac dysfunction, non-immune fetal hydrops, intravascular thrombosis, fetal hemorrhage, and intrauterine fetal demise [3,5]. Furthermore, excessive, closely approximated, low resistance vasculature can lead to arteriovenous malformation, which can further contribute to the development of hydropic changes and cardiac dysfunction [3]. Umbilical cord hemangiomas have also been associated, to varying degrees, with increased maternal serum alpha-fetoprotein levels, other vascular anomalies, polyhydramnios, and preterm birth [6].
Umbilical cord hemangiomas should be suspected when antenatal sonography reveals a hyperechoic mass with or without cystic features, often containing branching, low-resistance vessels [2]. Differential diagnoses include hematomas, varicose veins, aneurysms, thrombosis, abdominal wall hernia, omphalomesenteric duct cysts, allantoic cysts, and tumors such as teratoma and metastatic neuroblastoma [7]. The presence of blood flow on color Doppler with associated uterine artery hypoplasia or the presence of calcifications within the mass can help differentiate hemangioma from teratomas [4,5]. Three-dimensional imaging may improve the spatial orientation of the size, location, and internal characteristics of cord swelling [8].
In our literature review, 33 cases were identified prenatally at an average of 23.7 weeks gestation (Table 1) [2,4,5,7-36]. In the 28 cases that specified tumor location, umbilical cord hemangiomas were found within 10cm of the placenta in 50% of cases, within 10cm of the fetal insertion in approximately 40% of cases, and the remainder were in the mid-cord. These tumors were found to enlarge in nearly 40% of cases, and cystic structures were present in almost half. Umbilical cord hemangiomas are usually an isolated lesion, without major structural anomalies, however, they have been associated with vascular malformations. In our literature review, nearly 25% of umbilical cord hemangiomas were found in patients with cutaneous hemangiomas, visceral hemangiomas, and even Klippel-Trenaunay-Weber syndrome [9,11,18,20,22,30,32,34]. While umbilical cord hemangiomas have been associated with alterations in amniotic fluid, this was not often documented in the reports, and we identified oligohydramnios in 9%, and polyhydramnios in 15%. In cases identified prenatally, 40% resulted in preterm birth and 18% were found to have cardiac failure or dysfunction. In all, fetal survival was approximately 80%.
Study | GA | Location | Growth | Cysts | AFP | Amniotic fluid | Preterm birth | Hydrops / heart failure | Survival |
|---|---|---|---|---|---|---|---|---|---|
GA: gestational age at diagnosis; AFP: maternal alpha fetoprotein; Y: yes; N: no; NA: not available/applicable; oligo: oligohydramnios; poly: polyhydramnios; IUFD: intrauterine fetal demise; TOP: termination of pregnancy | |||||||||
Jauniaux 1990 | 20w | placenta | Y | Y | normal | N | none | Y | |
Ghidini 1990 | 34w | 10cm from fetal | N | Y | normal | N | Y | ||
Gramellini 1993 | 26w | placenta | N | poly | 36w | none | Y | ||
Weyerts 1993 | 33w | fetal | N | normal | N | Y | |||
Wilson 1994 | 17w | NA | Y | Y | oligo | 36w | Y | ||
Armes 1994 | 32w | 9cm from placenta | poly | 34w | N (perinatal) | ||||
Shipp 1995 | 33w | placenta | oligo | 36w | Y | ||||
Miller 1997 | 15w | fetal | ↑ | N | Y | ||||
Tennsteadt 1998 | 18w | fetal | Y | Y | normal | 36w | Y | ||
Kamitomo 2000 | 16w | placenta | Y | ↑ | NA | IUFD 17w | |||
Sahinoglu 2003 | 24w | NA | normal | 26w | N (perinatal) | ||||
Caldarella 2003 | 32w | placenta | normal | 32w | hydrops, cardiomegaly | Y | |||
Daniel-Spiegel 2005 | 27w | 10cm from placenta | Y | Y | normal | oligo | N | Y | |
Cheng 2006 | 19w | placenta | Y | ↑ | N | Y | |||
Iyoob 2006 | 30w | placenta | Y | poly | 30w | heart failure | Y | ||
Natalucci 2006 | 33w | fetal | ↑ | N | Y | ||||
Malliah 2007 | 19w | placenta | Y | poly | N | Y | |||
Papadopoulos 2009 | 22w | 22cm from placenta | Y | normal | 37w | Y | |||
Gouin 2009 | 25w | NA | normal | N | Y | ||||
Sathiyathasan 2010 | 22w | NA | NA | IUFD 26w | |||||
Matsuda 2011 | 18w | fetal | Y | Y | N | Y | |||
Hara 2015 | 26w | placenta | Y | ↑ | 29w | heart failure | Y | ||
Smulian 2016 | 25w | fetal | 36w | hydrops | Y | ||||
Akiba 2017 | 19w | fetal | N | Y | N | Y | |||
Rocha 2017 | 23w | NA | normal | N | Y | ||||
Schwickert 2018 | 38w | placenta | N | N | Y | ||||
Angelico 2019 | 34w | 20cm from placenta | Y | Y | 36w | Y | |||
Yu 2020 | 17w | fetal | N | Y | normal | NA | pericardial effusion | TOP | |
Zhang 2021 | 22w | placenta | Y | Y | 34w | Y | |||
Hadravská 2021 | 22w | placenta | N | normal | poly | NA | hydrops | IUFD 28w | |
Kaur 2022 | 13w | fetal | Y | Y | 33w | Y | |||
Lok 2022 | 21w | fetal | Y | NA | IUFD 21w | ||||
Lisovaja 2022 | 24w | mid-cord | Y | Y | N | Y | |||
The optimal management of a patient with cord swelling or mass is not clearly defined. Since 1990, serial surveillance has been suggested once a suspected umbilical cord hemangioma is detected on ultrasound [4]. Three decades later, there is no standard for frequency or type of antepartum assessment. Our patient underwent weekly ultrasound examinations and monitoring with biophysical profile. Despite progressive mass enlargement and development of polyhydramnios, there were no concerning findings in the cord vessel dynamics and no fetal distress. Upon detection of fetal cardiac changes at 31 weeks, we increased monitoring to twice weekly with non-stress testing and umbilical artery Doppler assessment. No flow abnormalities were detected and fetal cardiac findings stabilized. Despite a large mass confirmed at delivery, there were no variable decelerations in labor.
Umbilical cord hemangiomas should be suspected when a hyperechoic mass is found along the fetal umbilical cord. As a rare tumor with solid and pseudocystic changes, serious maternal and fetal complications may occur, including preterm birth and fetal demise. While labor may be tolerated, we recommend at least weekly ultrasound surveillance from the time of initial detection to monitor for enlargement, cord vessel compression, thrombus, hemorrhage, polyhydramnios, as well as fetal hydrops and cardiac dysfunction.
References
[1] Fan M, Skupski DW. Placental chorioangioma: literature review. J Perinat Med. 2014;42(3):273-279. doi:10.1515/jpm-2013-0170
[2] Iyoob SD, Tsai A, Ruchelli ED, et al. Large Umbilical Cord Hemangioma: Sonographic Features With Surgical Pathologic Correlation. J Ultrasound Med. 2006;25(11):1495-1498. doi:10.7863/jum.2006.25.11.1495
[3] Smulian JC, Sarno AP, Rochon ML, et al. The natural history of an umbilical cord hemangioma. J Clin Ultrasound. 2016;44(7):455-458. doi:10.1002/jcu.22346
[4] Ghidini A, Romero R, Eisen RN, et al. Umbilical cord hemangioma. Prenatal identification and review of the literature. J Ultrasound Med. 1990;9(5):297-300. doi:10.7863/jum.1990.9.5.297
[5] Lok WY, Law KM, Ho CL, et al. Prenatal diagnosis of umbilical cord hemangioma. Ultrasound Obstet Gynecol. 2022;59(3):392-393. doi:10.1002/uog.24755
[6] Iglesias-Deus A, Pérez-Muñuzuri A, Urisarri A, Bautista-Casasnovas A, Couce ML. Umbilical cord and visceral hemangiomas diagnosed in the neonatal period: A case report and a review of the literature. Medicine (Baltimore). 2016;95(42):e5196. doi:10.1097/MD.0000000000005196
[7] Natalucci G, Wisser J, Weil R, Stallmach T, Ulrich Bucher H. Your diagnosis? Umbilical cord tumor. Eur J Pediatr. 2007;166(7):753-756. doi:10.1007/s00431-006-0301-2
[8] Akiba Y, Miyakoshi K, Ochiai D, Kawaida M, Matsumoto T, Tanaka M. Umbilical cord hemangioma: Sonographic features by HDlive Flow. Eur J Obstet Gynecol Reprod Biol. 2018;221:195-196. doi:10.1016/j.ejogrb.2017.12.011
[9] Jauniaux E, Moscoso G, Chitty L, et al. An angiomyxoma involving the whole length of the umbilical cord. Prenatal diagnosis by ultrasonography. J Ultrasound Med. 1990;9(7):419-422. doi:10.7863/jum.1990.9.7.419
[10] Gramellini D, Pedrazzoli G, Sacchini C, et al. Color Doppler ultrasound in prenatal diagnosis of umbilical cord angiomyxoma. Case report. Clin Exp Obstet Gynecol. 1993;20(4):241-244.
[11] Weyerts LK, Jones MC, Grafe M, S et al. Umbilical cord haemangioma associated with an eruptive cutaneous haemangioma in a female infant. Prenat Diagn. 1993;13(1):61-64. doi:10.1002/pd.1970130109
[12] Wilson RD, Magee JF, Sorensen PHB, et al. In utero decompression of umbilical cord angiomyxoma followed by vaginal delivery. Am J Obstet Gynecol. 1994;171(5):1383-1385. doi:10.1016/0002-9378(94)90167-8
[13] Armes JE, Billson VR. Umbilical cord hemangioma associated with polyhydramnios, congenital abnormalities and perinatal death in a twin pregnancy. Pathology (Phila). 1994;26(2):218-220. doi:10.1080/00313029400169521
[14] Shipp T, Bromley B, Benacerraf B. Sonographically detected abnormalities of the umbilical cord. Int J Gynecol Obstet. 1995;48(2):179-185. doi:10.1016/0020-7292(94)02297-C
[15] Miller KA, Gauderer MWL. Hemangioma of the umbilical cord mimicking an omphalocele. J Pediatr Surg. 1997;32(6):810-812. doi:10.1016/S0022-3468(97)90625-4
[16] Tennstedt C, Chaoui R, Bollmann R, D et al. Angiomyxoma of the Umbilical Cord in One Twin with Cystic Degeneration of Wharton’s Jelly. A Case Report. Pathol - Res Pract. 1998;194(1):55-58. doi:10.1016/S0344-0338(98)80012-5
[17] Kamitomo M, Sueyoshi K, Matsukita S, et al. Hemangioma of the Umbilical Cord: Stenotic Change of the Umbilical Vessels. Fetal Diagn Ther. 1999;14(6):328-331. doi:10.1159/000020951
[18] Sahinoglu Z, Uludogan M, Delikara NM. Prenatal sonographic diagnosis of Klippel-Trenaunay-Weber syndrome associated with umbilical cord hemangioma. Am J Perinatol. 2003;20(1):1-6. doi:10.1055/s-2003-37950
[19] Caldarella A, Buccoliero AM, Taddei A, et al. Hemangioma of the Umbilical Cord: Report of a Case. Pathol - Res Pract. 2003;199(1):51-55. doi:10.1078/0344-0338-00354
[20] Daniel-Spiegel E, Weiner E, Gimburg G, et al. The association of umbilical cord hemangioma with fetal vascular birthmarks. Prenat Diagn. 2005;25(4):300-303. doi:10.1002/pd.1109
[21] Cheng HP, Hsu CY, Chen CP, et al. Angiomyxoma of the Umbilical Cord. Taiwan J Obstet Gynecol. 2006;45(4):360-362. doi:10.1016/S1028-4559(09)60262-X
[22] Malliah R, Shah V, Heller D. Umbilical cord hemangioma associated with multiple cutaneous hemangiomas in a newborn. Int J Gynecol Obstet. 2007;99(1):58-58. doi:10.1016/j.ijgo.2007.02.016
[23] Papadopoulos VG, Kourea HP, Adonakis GL, et al. A case of umbilical cord hemangioma: Doppler studies and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2009;144(1):8-14. doi:10.1016/j.ejogrb.2009.01.011
[24] Gouin K, Kingdom J, Keating S. A Giant Cord Hemangioma Diagnosed at 32 Weeks’ Gestation. J Obstet Gynaecol Can. 2009;31(8):695. doi:10.1016/S1701-2163(16)34268-2
[25] Sathiyathasan S, Jeyanthan K, Hamid R. Umbilical hemangioma: a case report. Arch Gynecol Obstet. 2011;283(1):15-17. doi:10.1007/s00404-010-1606-y
[26] Matsuda S, Sato Y, Marutsuka K, et al. Hemangioma of the Umbilical Cord with Pseudocyst. Fetal Pediatr Pathol. 2011;30(1):16-21. doi:10.3109/15513811003796920
[27] Hara K, Fukumura Y, Saito T, et al. A giant cord hemangioma with extramedullary hematopoiesis and elevated maternal serum human chorionic gonadotropin: a case report and review of the literature. Diagn Pathol. 2015;10(1):154. doi:10.1186/s13000-015-0385-y
[28] Smulian JC, Sarno AP, Rochon ML, et al. The natural history of an umbilical cord hemangioma. J Clin Ultrasound. 2016;44(7):455-458. doi:10.1002/jcu.22346
[29] Rocha A, Rodrigues M do C, Braga J. Umbilical Cord Hemangioma with Pseudocyst: An Exceptional Finding. Acta Médica Port. 2017;30(9):662-662. doi:10.20344/amp.9274
[30] Schwickert A, Seeger KH, Rancourt RC, et al. Prenatally detected umbilical cord tumor as a sign of diffuse neonatal hemangiomatosis. J Clin Ultrasound JCU. 2019;47(6):366-368. doi:10.1002/jcu.22689
[31] Angelico G, Spadola S, Ieni A, et al. Hemangioma of the umbilical cord with associated amnionic inclusion cyst: two uncommon entities occurring simultaneously. Pathologica. 2019;111(2):86. doi:10.32074/1591-951X-26-17-EC
[32] Yu D, Sun L, Chen T. Prenatal ultrasound diagnosis of Klippel-Trenaunay-Weber syndrome associated with umbilical cord hemangioma. J Clin Ultrasound. 2021;49(3):254-256. doi:10.1002/jcu.22896
[33] Zhang L, Delisle MF, Hendson G, et al. Umbilical cord hemangioma with significant cord edema. J Obstet Gynaecol Can. 2021 Jul 22;S1701-2163(21)00579-X.
[34] Hadravská Š, Ismailová H, Peteříková AS, Daumová M. Non-immune hydrops fetalis associated with two umbilical cord hemangiomas and vascular malformation of the transverse mesocolon. Case report. Cesk Patol. 2021;57(4):216-220.
[35] Kaur N, Heerema-McKenney A, Kollikonda S, et al. Changing Course of an Umbilical Cord Mass - Chasing the Diagnosis of Angiomyxoma. Pediatr Dev Pathol Off J Soc Pediatr Pathol Paediatr Pathol Soc. 2022;25(5):558-561. doi:10.1177/10935266221106910
[36] Lisovaja I, Franckevica I, Vedmedovska N. Large Angiomyxoma of the Umbilical Cord-Uncomplicated Rupture of Tumor Membranes at 32 Weeks of Gestation. Diagnostics. 2022;12(6):1339. doi:10.3390/diagnostics12061339
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Margarita Alvarez de la Rosa Rodríguez Spain Physician

Igor Yarchuk United States Sonographer

Larysa Gazarova United States Physician

belen garrido Spain Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Carlos Orellana Venezuela Physician

Mayank Chowdhury India Physician

Michaela Apostolou Germany Physician

filiz halici öztürk Turkey Physician

Vladimir Lemaire United States Physician

Tatiana Koipish Belarus Physician
CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician
Halil Mesut Turkey Physician

Suat İnce Turkey Physician
Liem Dang Le Viet Nam Physician

Muradiye YILDIRIM Turkey Physician
ALBANA CEREKJA Italy Physician

Selvanandhini Gopalasundaram India Physician
SAMUEL GELVEZ TELLEZ Colombia Physician

Murat Cagan Turkey Physician
Eslam Adel ammar Egypt Physician
Mária Brešťanská Slovakia Physician
Rasha Abo Almagd Egypt Physician

Ionut Valcea Romania Physician
Đặng Mai Quỳnh Viet Nam Physician

Halil Korkut Dağlar United States Physician
KHALED RAMADAN Egypt Physician

Sumit Singhania India Radiologist

Dr Monika Sharma India Physician

Martina Vagaská Slovakia Physician

Annette Reuss Germany Physician

Tina Wade United States Sonographer
Mequanint Melesse Bicha Ethiopia Physician

Nguyen Xuan Cong Viet Nam Physician
Deniz OLUKLU Turkey Physician

Mai Phương Viet Nam Physician

Yogesh Chinnawar India Physician

Andrea Bernathova Slovakia Physician

mohamed ateya Egypt Physician
shay kevorkian Israel Physician

Manjula Budidapadu India Physician

Mahmoud Moussa United Kingdom Physician