Case of the Week #578
Turkey
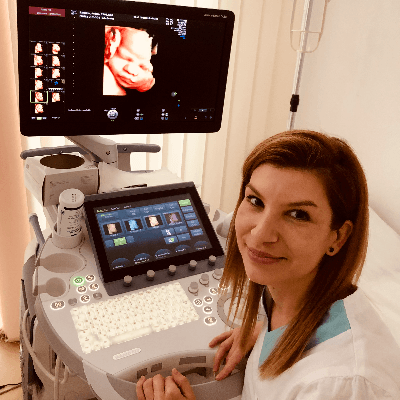
Case Report: 34-year-old woman in her 5th pregnancy presents for routine ultrasound examination at 23 weeks gestation.





View the Answer Hide the Answer
Answer
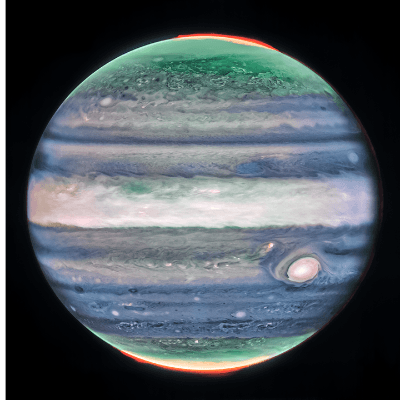
We present a case of epidermal cyst found on the scalp. The diagnosis was confirmed after birth (Image 1,2).


Introduction
Fetal scalp cysts are rare and the diagnosis is not always clear. Epidermal and dermoid cysts, which are fluid-filled benign masses, can be difficult to distinguish from neuroectodermal cysts, which may be associated with neurologic disability [1-3]. The first prenatal diagnosis of a scalp dermoid cyst was in 1998 [4].
Pathogenesis
Epidermal cysts are thought to arise from the displacement of epithelial nests as the neural pore closes in the early weeks of embryogenesis. Cysts can be found in the frontal and occipital regions. The fact that the majority of the lesions are in the midline suggests that it is a closure defect [4,5].
Differential diagnosis
When considering the germ cell layer from which the structure originates, the differential diagnosis of fetal scalp cysts includes:
- Epidermal and dermoid cysts derived from the ectoderm
- Lipomas, lymphangiomas, and hemangiomas derived from the mesoderm
- Meningoceles, meningomyeloceles, and encephaloceles derived from the neuroectoderm [3,5,6].
If a skull defect is not found on ultrasound or MRI imaging, other diagnoses within the differential include cystic hygroma, hamartoma, hematoma, and scalp edema [4,5,7]. Rarely, a sequestered meningocele, also known as extracranial meningeal heterotopia, can present as a cyst without a bony defect. It is thought that these lesions initially communicated through a defect in the skull which subsequently closed. These lesions are normally very vascular [5-7].
Sonographic diagnosis
While the diagnosis of epidermal cysts can be difficult, technological developments with high resolution transvaginal ultrasound, 3D ultrasound [3,5,7], and prenatal MRI [4] can be helpful in establishing the correct diagnosis. An epidermal cyst appears as an extracranial cystic or heterogeneous mass. The most reliable parameter for diagnosis is the absence of a defect in the calvarium. Small defects can be difficult to identify especially if the fetal position is not optimal. Both cranial suture lines and acoustic artifacts can be misinterpreted as bony defects [4]. Multiple images should be obtained at different angles to confirm a true defect in the skull [2,7]. An epidermal cyst is usually an isolated finding with no associated anomalies. During pregnancy, the mass tends to remain cystic, but regression of the lesion has also been reported [5].
Epidermal cysts are a diagnosis of exclusion. The central nervous system should be carefully examined to identify the presence of ventriculomegaly, abnormal head shape such as lemon sign or banana sign, obliteration of the cisterna magnum, or distortion of the cerebellum which can suggest the diagnosis of an encephalocele or meningocele [2,5]. Other findings associated with cephaloceles include agenesis of the corpus callosum, limb dysplasia, facial anomalies and urogenital anomalies, as in Meckel-Gruber syndrome. A high maternal or amniotic fluid alpha fetoprotein may suggest an open neural tube defect [2]. Color Doppler can be used to identify a vascular hemangioma or small feeding vessels through a bone defect in an encephalocele [2,3].
Management
To determine whether the calvarium has a defect is crucial in properly identifying a benign epidermal cyst [2]. Errors in the diagnosis have led to termination of pregnancy for this benign diagnosis [1]. Conversely, a fetus with neuroectodermal cyst may have neurologic disabilities, cerebrospinal fluid disturbances, or hydrocephalus. Once a prenatal diagnosis of an epidermal cyst is made, no further intervention is required. Mode of delivery should proceed according to obstetric indications. The cyst may require surgical excision after birth.
When a definitive diagnosis cannot be made prenatally, counselling is difficult. While encephaloceles are associated with poor neurologic outcomes, meningoceles located in the occiput, small lesions, absence of brain tissue in the herniation sac, and the absence of hydrocephalus are good prognostic signs, and associated with little or no physical and functional disability [2] Close observation of these lesions may ultimately lead to a positive outcome [3,7].
References
[1] Ferriman EL, McCormack J. An epidermal scalp cyst simulating an encephalocele. Prenat Diagn. 1995 Oct;15(10):981-2.
[2] Lau TK, Leung TN, Leung TY, et al. Fetal scalp cysts: challenge in diagnosis and counseling. J Ultrasound Med. 2001 Feb;20(2):175-7.
[3] Timor-Tritsch IE, Monteagudo A, Santos R. Fine-tuning the diagnosis of fetal scalp cysts: the value of high-frequency sonography. J Ultrasound Med. 2008 Sep;27(9):1363-8.
[4] Shahabi S, Busine A. Prenatal diagnosis of an epidermal scalp cyst simulating an encephalocoele. Prenat Diagn. 1998 Apr;18(4):373-7.
[5] Bae JY, Seong WJ, Lee TH, et al. Prenatal diagnosis of scalp cyst with spontaneous regression. J Clin Ultrasound. 2011 Oct;39(8):484-6.
[6] Ogle RF, Jauniaux E. Fetal scalp cysts--dilemmas in diagnosis. Prenat Diagn. 1999 Dec;19(12):1157-9.
[7] Sepulveda W, Wong AE, Sepulveda S, et al. Fetal scalp cyst or small meningocele: differential diagnosis with three-dimensional ultrasound. Fetal Diagn Ther. 2011;30(1):77-80.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Danilo Feitosa Brazil Physician

Umber Agarwal United Kingdom Maternal Fetal Medicine

Igor Yarchuk United States Sonographer

Larysa Gazarova United States Physician

belen garrido Spain Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Carlos Orellana Venezuela Physician

Mayank Chowdhury India Physician

Michaela Apostolou Germany Physician
Adrian Popa Romania Physician

Vladimir Lemaire United States Physician
Ivan Ivanov Russian Federation Physician

Boujemaa Oueslati Tunisia Physician

Tatiana Koipish Belarus Physician
CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician
Halil Mesut Turkey Physician
Emiliano Ciari Argentina Physician

Suat İnce Turkey Physician
Shari Morgan United States Sonographer

Elena Andreeva Russian Federation Physician

Muradiye YILDIRIM Turkey Physician

Dimitrios Spiliopoulos Greece Physician

doğa öcal Turkey Physician

ALBANA CEREKJA Italy Physician

Selvanandhini Gopalasundaram India Physician
Eti Zetounie Israel Sonographer

Murat Cagan Turkey Physician

Umutcan KAYIKÇI Turkey Physician
Mária Brešťanská Slovakia Physician
Rasha Abo Almagd Egypt Physician

Ionut Valcea Romania Physician

Halil Korkut Dağlar United States Physician

Prakriti Patil India Physician
KHALED RAMADAN Egypt Physician

Borisova Elena Russian Federation Physician

Kathrine Montagne United States Sonographer
CHANDRAKANTH K S India Physician

Dr Monika Sharma India Physician
Martina Vagaská Slovakia Physician

Hannah Danielson United States Sonographer

Mariam Bamanie Saudi Arabia Physician
Fred Pop Uganda Sonographer

Vandana Yakub India Physician
Mequanint Melesse Bicha Ethiopia Physician

Nguyen Xuan Cong Viet Nam Physician
Deniz OLUKLU Turkey Physician

Mai Phương Viet Nam Physician

Yogesh Chinnawar India Physician

vaibhav jaiswal India radiologist

Samy Zandoná Brazil Physician

Andrea Bernathova Slovakia Physician

Katherine Gorman United States Sonographer

mohamed ateya Egypt Physician

Poojitha Alladi India Physician
shay kevorkian Israel Physician

Dr.Annette Reuss Germany Physician

Kimberly Dailey United States Sonographer