Case of the Week #573
(1) Femicare, Center of prenatal ultrasonographic diagnostics, Martin, Slovakia; (2) St Mary's Medical Center, San Francisco, CA, USA
Case Report: A 31-year-old G2P1 presented to our office at 28 weeks, 5 days due to fetal cardiac enlargement. Her 8-year-old son was monitored due to a “large heart” after delivery, but the finding resolved and he is doing well. During the pregnancy, serologic testing for Toxoplasmosis was negative. Additionally, the mother was infected with COVID at 10 weeks gestation without any complications.
Ultrasonographic examination at 20 weeks was reported to be normal without any cardiac anomalies. However, due to the family history of transient cardiac enlargement in her first child, the patient was sent to the National Institute for Cardiovascular Diseases in the Slovak Republic at 25 weeks gestation where fetal cardiomegaly and possible ventricular septal defect were found.
At 28 weeks, 5 days the patient visited our office, and our examination revealed following findings:

View the Answer Hide the Answer
Answer
We present a case of dissecting aneurysm of the interventricular septum.
The baby was born at 34 weeks, 6 days by cesarean section due to polyhydramnios and worsening flow parameters in the umbilical arteries and middle cerebral artery. While there was suspicion of fetal anemia, this was not confirmed after delivery. A female infant (birth weight 2390g, length 45 cm, Apgar 4/7) was born hypotonic, apneic, bradycardic, and required nasal continuous positive airway pressure ventilation. The baby was admitted to the cardiac neonatal intensive care unit due to cardiomegaly and hemodynamic decompensation.
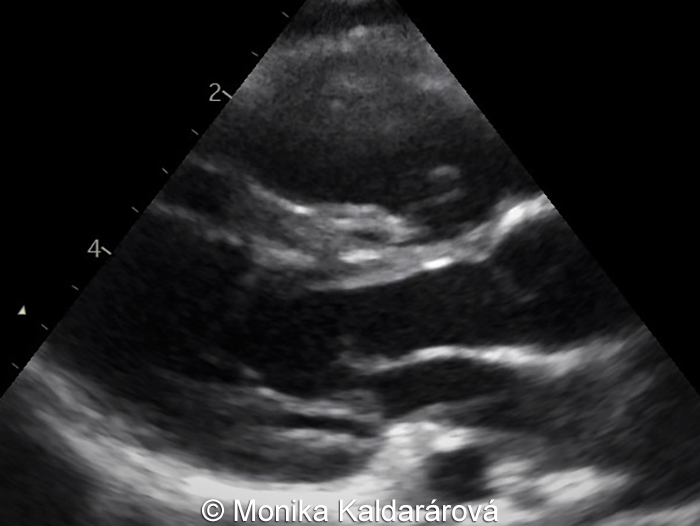
Postnatal sonography revealed dilated cardiomyopathy with abnormal septum and defective septal myocardium. The septum was not contracting and bulged to both the right and left sides during the cardiac cycle, with predominant compression of the left ventricle. ECG showed first degree atrioventricular block, and right bundle branch block.
A couple of days later, the echocardiographic appearance of the heart had changed, and was described as concentric hypertrophic cardiomyopathy affecting both ventricles without left outflow tract obstruction. There was systolic dysfunction of the right ventricle and mild systolic dysfunction of the left ventricle (Image 1). Metabolic tests were normal. A genetic study evaluating 128 genes relevant to cardiomyopathies did not find any anomalies.
Ten months later, ultrasonographic examinations showed normal function of both ventricles (Image 2). At the time of this publication, the baby is 14 months old and is doing well. The cardiac finding has improved, and the heart has nearly a normal appearance.

The ultrasound findings are demonstrated in the following images, videos and figures.
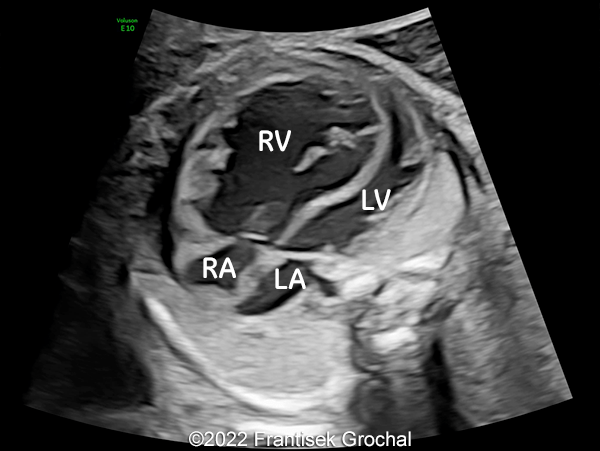
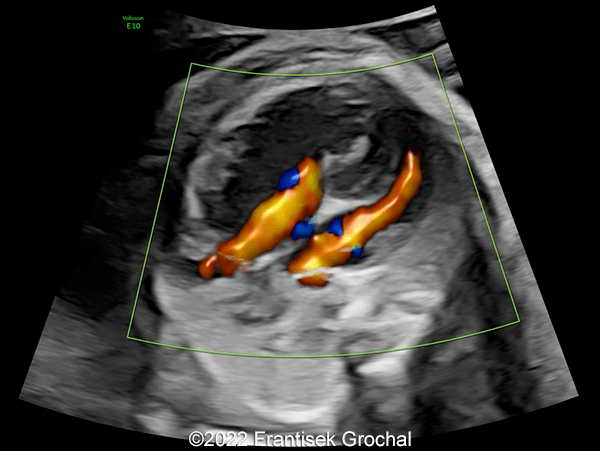
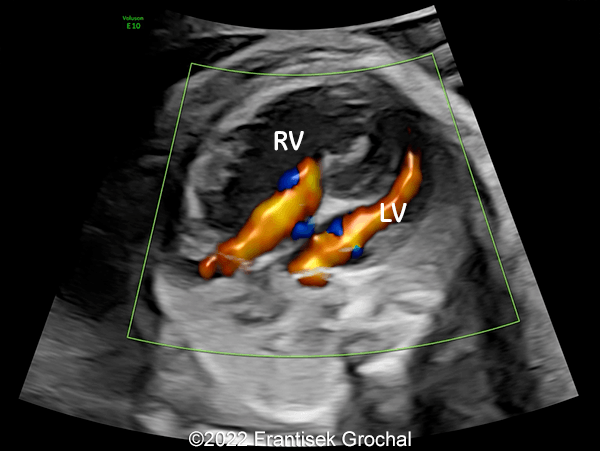
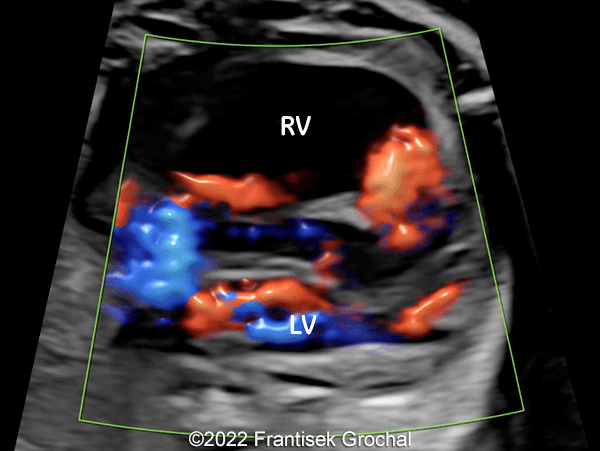
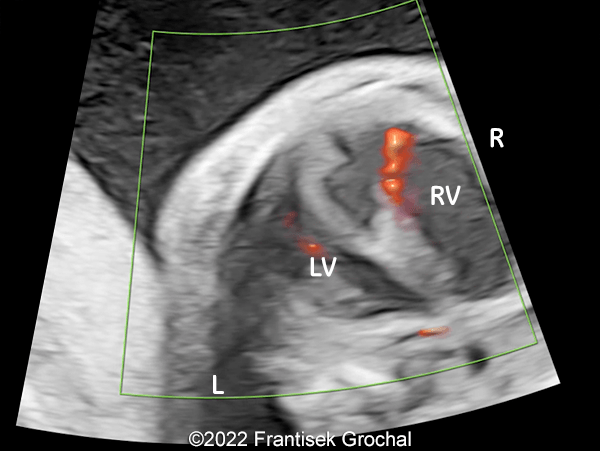
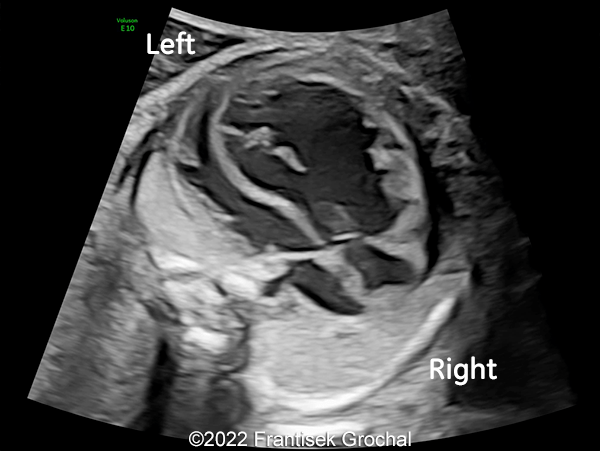
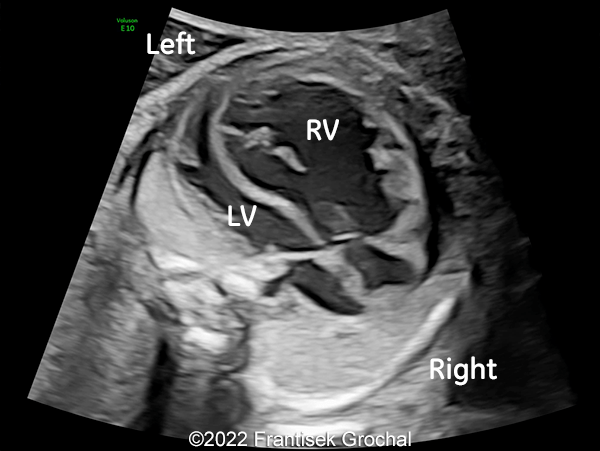
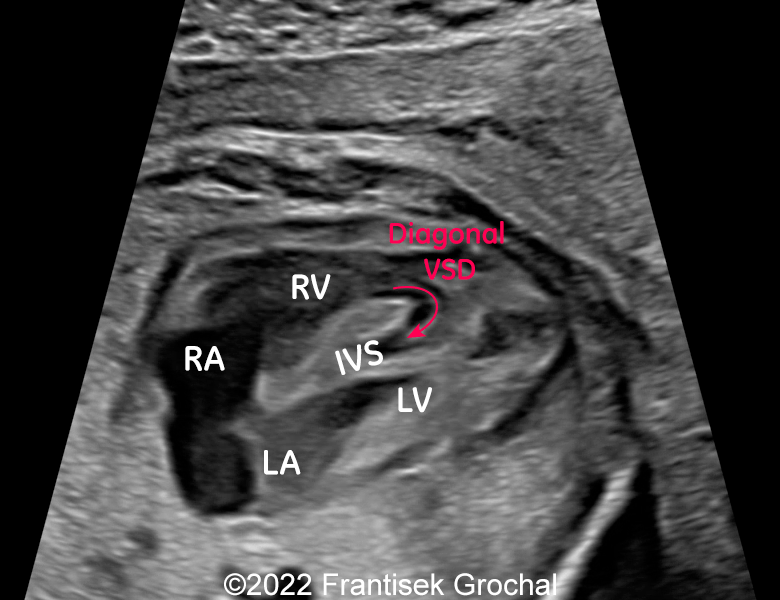
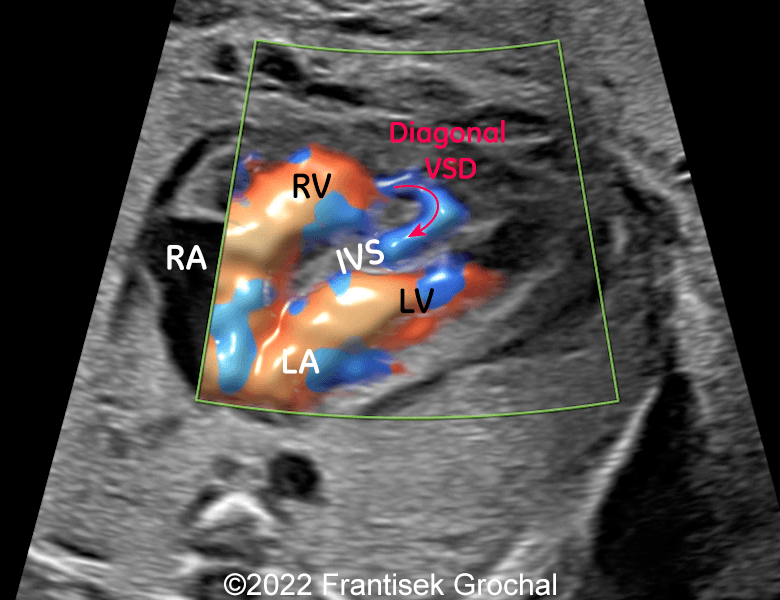
Images 3-5 and Video 1, 2 show a four-chamber view of the heart. The heart is enlarged with dilated ventricles, predominantly affecting the right side. The interventricular septum (IVS) of the heart has an abnormal appearance with a central cavity and separation of the left and right walls. A defect can be seen in the right wall close to the apex. During the cardiac cycle, blood flows in and out of the abnormal interventricular septal cavity through the defect in the right wall (depicted by white curved arrows in Images 3-5). Blood flowing into the septum dissects its walls, and the left wall of the septum bulges into the left ventricle, obstructing the outflow tract. These structural changes are responsible for worsening cardiac function with diminished ejection fraction and dilated cardiomyopathy.
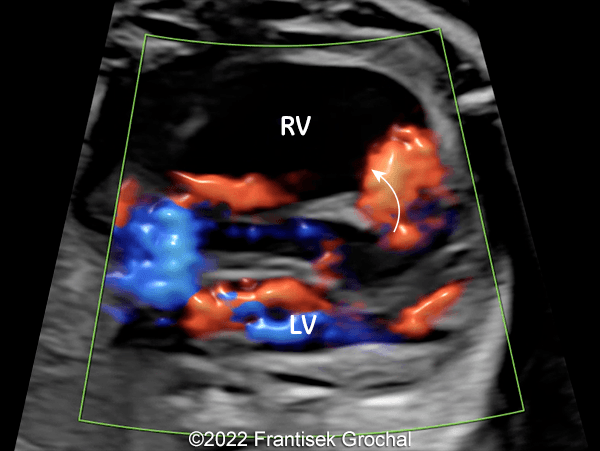
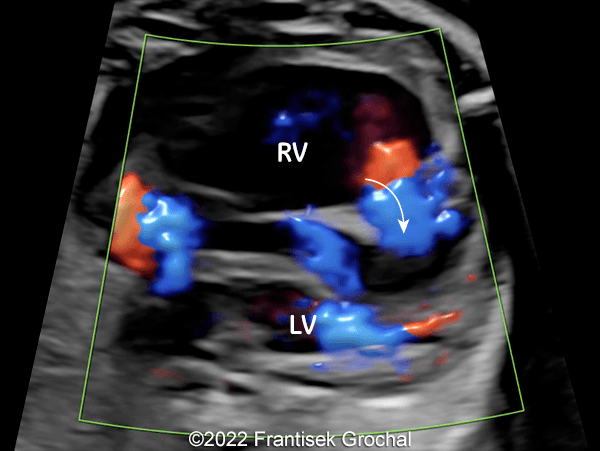
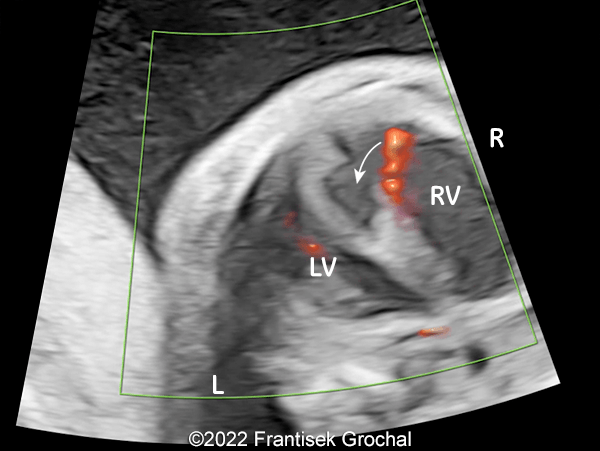
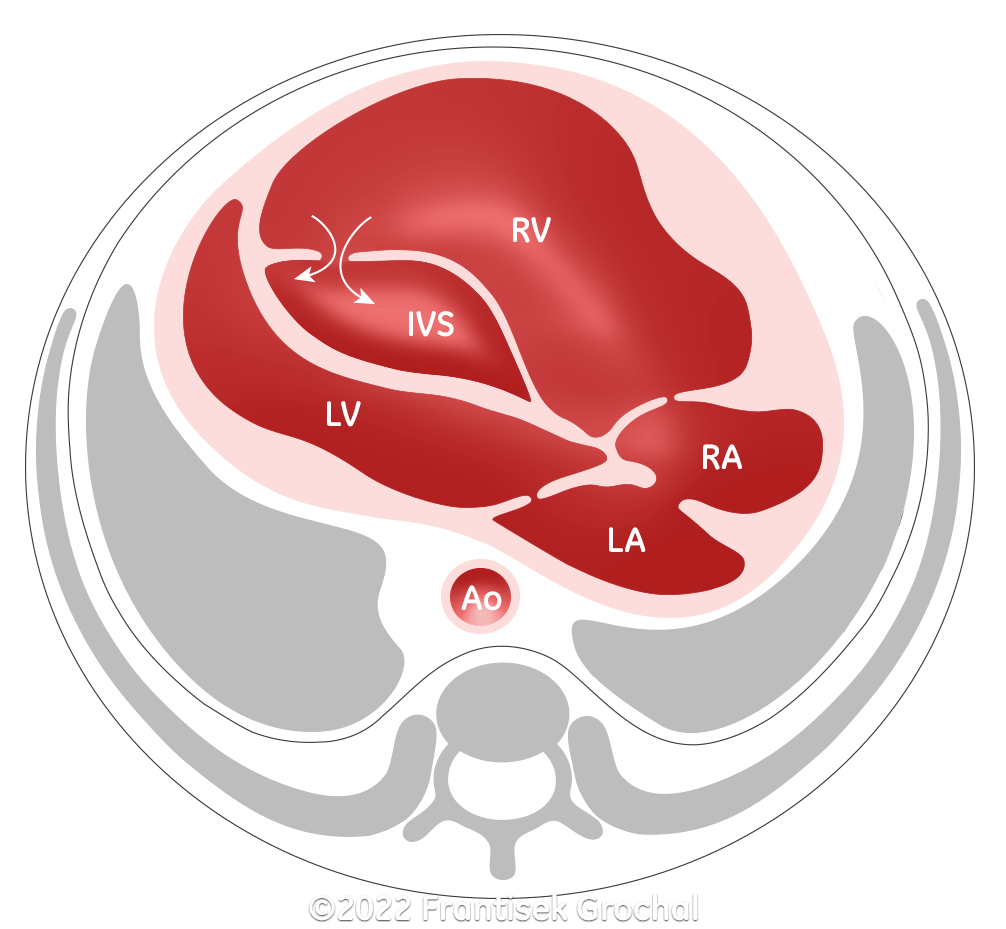
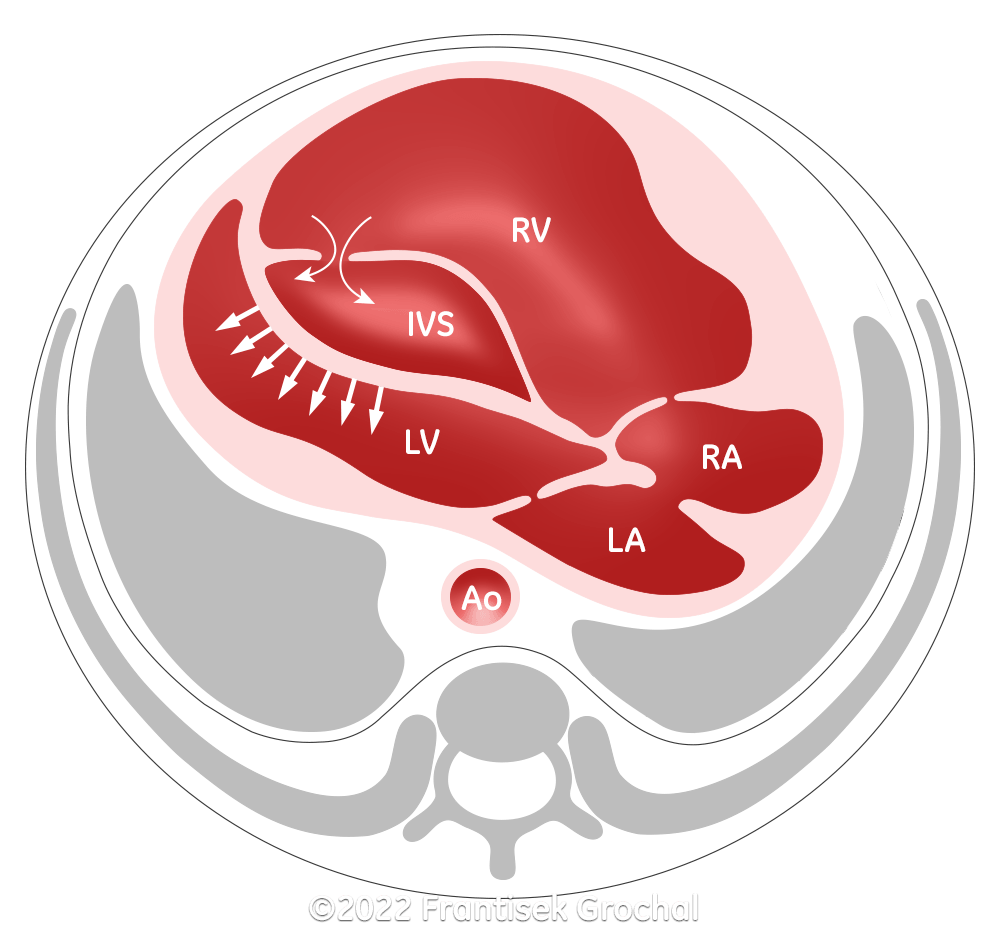
Image 6 caption: Diagram demonstrating the dissecting aneurysm of the interventricular septum seen in our case. There is a defect in the right wall of the septum which allows blood flow into the interventricular septum. (RV–right ventricle; LV–left ventricle; IVS–interventricular septum; RA–right atrium; LA–left atrium; Ao–aorta)
Discussion
Congenital ventricular aneurysms are broad-based bulges in the ventricular wall with noncontractile, or dyskinetic myocardium [1]. While in the postnatal period, a ventricular aneurysm can be acquired as a complication of surgical procedures [2], trauma [3], Kawasaki disease [4], infection [4], or following a myocardial infarction [6], congenital aneurysms have no clear causative factor. In contrast, a congenital ventricular diverticulum is a fingerlike pouch with a narrow connection to the ventricle that contains epicardium, myocardium, and endocardium on histology, and contracts either normally or near normally [1]. On prenatal imaging, it can be difficult to distinguish between ventricular aneurysms and diverticula [1]. Given their rarity, the prevalence of ventricular diverticula and aneurysms is difficult to estimate. A study reviewing 12,924 consecutive autopsies in children found 750 cases with congenital cardiac defects and only 3 cases of ventricular diverticula (23 in 100,000 cases) [7]. A more recent publication in 12,271 consecutive adult patients undergoing coronary angiography demonstrated a prevalence of 76 in 10,000 cases of congenital left ventricular aneurysm and diverticula [8]. The etiology of congenital ventricular aneurysms is not known, though may be related to prenatal ischemia leading to aneurysm formation [9], connective tissue disorders in patients with Ehlers-Danlos syndrome [10], or a genetic defect in mesenchymal cell migration in patients with familial occurrence [11,12].
Congenital ventricular aneurysms are more commonly located in the apex and anterolateral wall of the ventricle [8], and are rarely found in the interventricular septum. In ventricular septal aneurysms, the abnormal tissue can involve the membranous or muscular portion of the septum [13]. In cases involving the membranous portion of the ventricular septum, aneurysms may represent a mechanism for spontaneous closure of ventricular septal defects [14].
Congenital aneurysms of the muscular intraventricular septum are extremely rare. There have been 22 cases reported in the literature (Table 1) [11,13,15-29], 10 of which were diagnosed prenatally. Approximately 75% (16) of cases had associated cardiac anomalies, most commonly ventricular septal defect (7) located either in the perimembranous septum or in the aneurysm, atrial septal defect (5), and right heart lesions (5) such as pulmonary atresia with tricuspid valve stenosis and right ventricular aneurysm. Patients rarely presented with extracardiac anomalies. While 55% (12) of patients were asymptomatic, rhythm disturbances such as first-degree atrioventricular block, right bundle branch block, and Wolf-Parkinson-White occurred in 18% (4), and symptoms of congestive heart failure occurred in another 18% (4). Seven cases were treated surgically, though only 3 cases required plication or resection of the aneurysm, and the remainder underwent surgical treatment of concomitant cardiac structural defects. Survival was approximately 90% with one termination of pregnancy and one death. Follow up extended anywhere between 3 months and 12 years.
In patients with congenital muscular interventricular septal defect, there have been several familial cases, suggesting an autosomal dominant inheritance with variable expressivity [11,27,28]. Of the 22 cases reported in the literature, 32% (7) mentioned a family history of heart disease. Development of a muscular interventricular septal defect may be a result of a genetic mutation in mesenchymal cell migration from the atrioventricular and conotruncal regions to the cephalic portion of the developing interventricular septum [11,12]. Alternatively, a muscular septal aneurysm may be a result of ischemia or embolism [22]. In our literature review, 13 cases documented the coronary artery anatomy, 9 of which were normal, 3 showed right ventricular sinusoids associated with pulmonary atresia, and one showed abnormal circumflex artery distribution.
Study | Prenatal DX | Age | Symptoms | Cardiac findings | Cardiac rhythm | Coronary circulation | Associated anomalies | treatment | Family history | Survived |
|---|---|---|---|---|---|---|---|---|---|---|
Abbreviations: ASD: atrial septal defect; AV: atrioventricular; Dx: diagnosis; LCA: left coronary artery; LBBB: left bundle branch block; NA: not available; NSR: normal sinus rhythm; m: months; PA: pulmonary atresia; PDA: patient ductus arteriosus; RBBB: right bundle branch block; RV: right ventricle; SOB: shortness of breath; TOP: termination of pregnancy; VSD: ventricular septal defect; VT: ventricular tachycardia; w GA: weeks gestational age; y: years | ||||||||||
Baspinar 2005 | no | 5m | none | ASD | Wolf-Parkinson-White | normal | no | none | no | yes |
Chen 1991 | no | 4y | none | none | NSR | NA | no | none | yes | yes |
Edelstein 1965 | no | 8y | none | VSD | incomplete RBBB | NA | no | none | NA | yes |
Eriksson 1998 | no | 7y | none | ASD | NSR | normal | no | none | yes | yes |
Eriksson 1998 | no | 5y | none | none | NSR | normal | no | none | yes | yes |
Fasoli 1988 | no | 15y | exertional dyspnea | ASD, mitral valve cleft | VT | normal | no | surgery- ASD | NA | yes |
Magherini 1988 | no | 10y | none | VSD | abnormal R wave progression, ST-T changes consistent with septal MI | normal | no | none | NA | yes |
Mohan 1992 | no | 18y | none | VSD | NSR | NA | no | none | NA | yes |
Nguyen 2008 | no | neonate | NA | pulmonary atresia, tricuspid stenosis, VSD | NA | single LCA, multiple RV sinusoids | NA | surgery-PA, aneurysm plication | NA | yes |
Nguyen 2022 | no | 18m | none | none | 1st degree AV block, RBBB | normal | no | none | no | yes |
Prabhakar 1993 | no | 1y | SOB with feeding | VSD | NSR | normal | no | surgery-aneurysm resection | NA | yes |
Wong 2007 | no | neonate | poor feeding | PDA | LBBB, RBBB | NA | chromosome 20 | none | NA | yes |
Carr 2008 | yes | 19w GA | diaphoresis with feeding | none | NSR | normal | no | cardiac transplant | no | yes |
Donofrio 2002 | yes | 26w GA | none | ASD | nonspecific ST segment and T wave abnormality | abnormal circumflex artery distribution | no | medical | yes | yes |
Fujiwara 2001 | yes | 26w GA | none | none | NSR | NA | no | none | yes | yes |
Fujiwara 2001 | yes | 28w GA | none | ASD, VSD | NSR | NA | no | none | yes | yes |
Ivanitskaya 2017 | yes | 22w GA | NA | hypoplastic aortic arch, VSD | NA | NA | hydrocephaly | NA | no | TOP |
Nguyen 2008 | yes | 28w GA | NA | pulmonary atresia, tricuspid stenosis, cleft mitral valve | NA | multiple RV sinusoids | NA | surgery-PA | NA | yes |
Nguyen 2008 | yes | 23w GA | NA | pulmonary atresia, tricuspid stenosis, | NA | multiple RV sinusoids | NA | surgery-PA | NA | yes |
Nguyen 2008 | yes | 28w GA | NA | absent pulmonary valve, tricuspid stenosis, PDA | NA | NA | NA | none | NA | no |
Nicholae 2007 | yes | NA | cyanosis | none | NA | normal | no | surgery-aneurysm resection | yes | yes |
Ozkavukcu 2018 | yes | 22w GA | none | RV aneurysm | no arrythmias | NA | no | none | NA | yes |
Our case more specifically represents a dissecting aneurysm of the interventricular septum. There are several reports in adults with a prevalence of 1.6 to 19.5 in 100,000 cases [30, 31]. While acquired lesions are a result of myocardial infarction, cardiac surgery, or endocarditis [30], an aneurysm of the sinus of Valsalva is a common etiology of an interventricular septal dissection [30, 31]. The mechanism is thought to be a result of compression of the coronary artery by the aneurysm of the coronary sinus of Valsalva leading to ventricular septal ischemia [32]. In cases with dissecting interventricular aneurysm, approximately 90% had an aneurysm that originated in the right coronary sinus of Valsalva [33].
This is the first case of dissecting aneurysm of the interventricular septum identified prenatally. Six cases have been reported in children, five of which were in adolescents [33-38]. These all originated from a right sinus of Valsalva aneurysm except for one in which there was no communication found between the dissecting interventricular aneurysm and the sinus of Valsalva (38). Similarly, two cases documented by Wu et al had normal sinuses of Valsalva, suggesting there may be other causes of this condition [31]. In our case, we hypothesize that a partial rupture of the interventricular aneurysm may lead to bleeding into the interventricular septum with dissection of the interstitium. The diagonal course of the defect through the interventricular septum may be a predisposing factor for the dissection (Image 8-9, Video 3-4).
While adult and adolescent patients with interventricular septal dissection may have significant anatomic and hemodynamic derangements leading to arrhythmias or congestive heart failure and necessitating surgery [30, 31, 33-37], there is no data to understand the natural history in fetal and neonatal life. Aneurysms of the membranous portion of the ventricular septum can be associated with complications such as cerebral infarction secondary to embolism [39], and right ventricular outflow obstruction [40]. In our literature review, muscular aneurysms can lead to conduction abnormalities [15, 17, 22, 24], and congestive heart failure [18, 23, 25, 28], though several cases documented improvement of the interventricular septal findings on serial echocardiography likely due to ventricular remodeling [22, 24, 29]. This was the case in our patient with a favorable outcome of the pregnancy and delivery, and gradual improvement of the cardiac findings. Due to lack of data, counselling patients can be a challenge, though lack of cardiac failure, such as fetal hydrops, or pericardial effusion could be a favorable predictive sign.
References
[1] Morin C, Ponzio A, Guirgis M, et al. Prenatal diagnosis of congenital ventricular aneurysm and diverticulum: Prenatal features and perinatal management. Prenat Diagn. 2022 Apr;42(4):428-434.
[2] Weesner KM, Byrum C, Rosenthal A. Left ventricular aneurysms associated with intraoperative venting of the cardiac apex in children. Am Heart J 1981;101:622–5
[3] Veeragandham RS, Backer CL, Mavroudis C, et al. Traumatic left ventricular aneurysm and tricuspid insufficiency in a child. Ann Thorac Surg 1998;66:247–8.
[4] Menahem S, Lefkovits J. Major Complication Following Kawasaki Disease in an Infant-The Development of Apical Infarction and Aneurysm Formation. Children (Basel). 2021 Oct 29;8(11):981.
[5] Arora K, Das RR, Tandon R, et al. Pseudoaneurysm of Left Ventricle following Staphylococcal Pericarditis in a Child. APSP J Case Rep. 2015 Sep-Dec; 6(3): 26.
[6] Kothari SS, Roy A, Sharma G. Left ventricular pseudoaneurysm in a child. Heart 2005;91:773.
[7] Albrecht G. [Morphology and formal etiology of congenital heart diverticula]. Zentralbl Allg Pathol. 1972;116(1):42-7.
[8] Ohlow MA, Secknus MA, Geller JC, et al. Prevalence and outcome of congenital left ventricular aneurysms and diverticula in an adult population. Cardiology. 2009;112(4):287-93.
[9] Patel CR, Judge NE, Muise KL, et al. Prenatal myocardial infarction suspected by fetal echocardiography. J Am Soc Echocardiogr. 1996 Sep-Oct;9(5):721-3.
[10] Mishra M, Chambers JB, Grahame R. Ventricular septal aneurysm in a case of Ehlers-Danlos syndrome. Int J Cardiol. 1992 Sep;36(3):369-70.
[11] Eriksson H, Cooper SM, Rosenbaum KN, et al. Familial occurrence of congenital aneurysm of the muscular interventricular septum. Pediatr Cardiol. 1998 May-Jun;19(3):249-52.
[12] Strauss M, Arrechedera H, Arguello C et al. Mesenchymal tissue of the interventricular septum. Structural and ultrastructural study. Anat Embryol (Berl). 1987;176(2):231-7.
[13] Ivanitskaya O, Andreeva E, Odegova N. Two Cases of Prenatally Diagnosed Membranous and Muscular Ventricular Septal Aneurysms. J Ultrasound Med. 2018 Apr;37(4):1039-1042.
[14] Miyake T, Shinohara T, Nakamura Y, et al. Aneurysm of the ventricular membranous septum: serial echocardiographic studies. Pediatr Cardiol. 2004 Jul-Aug;25(4):385-9
[15] Başpinar O, Karaaslan S, Oran B, et al. Congenital aneurysm of the muscular interventricular septum in a child. Turk J Pediatr. 2005 Jan-Mar;47(1):82-4.
[16] Chen MR, Rigby ML, Redington AN. Familial aneurysms of the interventricular septum. Br Heart J. 1991 Feb; 65(2): 104–106.
[17] Edelstein J, Charms BL. Ventricular septal aneurysms. A report of two cases. Circulation. 1965 Dec;32(6):981-4.
[18] Fasoli G, Valentina PD, Scognamiglio R. Echocardiographic findings in left ventricular septal aneurysm. Int J Cardiol. 1988 Mar;18(3):441-3.
[19] Magherini A, Schmidtlein C, Urciuolo A, et al. Congenital aneurysm of the interventricular muscular septum with rupture into the right ventricle in a child. Am Heart J. 1988 Jul;116(1 Pt 1):185-7.
[20] Mohan JC, Kumar P. Cross-sectional echocardiographic diagnosis of a congenital aneurysm of the muscular interventricular septum. Int J Cardiol. 1992; 35(3):415-416.
[21] Nguyen TP, Srivastava S, Ko HH, et al. Congenital muscular ventricular septal aneurysm: report of four cases and review of the literature. Pediatr Cardiol. 2008 Jan;29(1):40-4.
[22] Nguyen HH, Jay PY. Congenital Aneurysm of the Muscular Interventricular Septum Associated With Bifascicular Block. Cureus 2022 Oct;14(10): e29994.
[23] Prabhakar G, Kumar N, al-Oufi S, et al. Congenital aneurysm of the muscular interventricular septum. Eur Heart J. 1993 Sep;14(9):1294-6.
[24] Wong SH, Coleman DM, Aftimos S. Congenital aneurysm of the muscular interventricular septum in association with cardiac arrhythmias and a chromosomal abnormality. Pediatr Cardiol. 2007 Jan-Feb;28(1):57-60.
[25] Carr M, Kearney DL, Eidem BW. Congenital aneurysm of the muscular interventricular septum. J Am Soc Echocardiogr. 2008 Nov;21(11):1282.e1-6.
[26] Donofrio MT, Allen DR, Tekin M et al. Autosomal dominant myocardial disease diagnosed by fetal presentation of proband with an aneurysm of the muscular interventricular septum. Pediatr Cardiol. 2002 Jan-Feb;23(1):27-31.
[27] Fujiwara M, Sase M, Kondou O, et al. Congenital aneurysm of the muscular interventricular septum in a fraternal case diagnosed by fetal echocardiography. Pediatr Cardiol. 2001 Jul-Aug;22(4):353-6.
[28] Nicolae MI, Summers KM, Radford DJ. Familial muscular ventricular septal defects and aneurysms of the muscular interventricular septum. Cardiol Young. 2007 Oct;17(5):523-7.
[29] Ozkavukcu E, Babaturk A, Haliloglu N, et al. Concurrent Septal and Right Ventricular Aneurysms Detected on Second Trimester Ultrasound Scan: A Case Report. Eurasian J Med. 2018 Feb;50(1):50-52.
[30] Gu X, He Y, Luan S, et al. Dissection of the interventricular septum: Echocardiographic features. Medicine (Baltimore). 2017 Mar;96(10):e6191.
[31] Wu Q, Xu J, Shen X, et al. Surgical treatment of dissecting aneurysm of the interventricular septum. Eur J Cardiothorac Surg. 2002 Oct;22(4):517-20.
[32] Gallet B, Combe E, Saudemont JP, et al. Aneurysm of the left aortic sinus causing coronary compression and unstable angina: successful repair by isolated closure of the aneurysm. Am Heart J. 1988 Jun;115(6):1308-10.
[33] Choudhary SK, Bhan A, Reddy SC, et al. Aneurysm of sinus of Valsalva dissecting into interventricular septum. Ann Thorac Surg. 1998 Mar;65(3):735-40.
[34] Atiq M, Ali F, Hasan SB. Dissecting aneurysm of the interventricular septum due to rupture of the sinus of Valsalva. Cardiol Young. 2017 Apr;27(3):609-612.
[35] Barik R, Nemani L, Mishra RC. Giant unruptured sinus of Valsalva aneurysm with complete heart block. J Cardiol Cases. 2015 Oct 21;13(1):17-20.
[36] Engel PJ, Held JS, van der Bel-Kahn J, et al. Echocardiographic diagnosis of congenital sinus of Valsalva aneurysm with dissection of the interventricular septum. Circulation. 1981;63(3):705–711.
[37] Math RS, Saxena A, Chakraborty P, et al. An unusual case of dissecting aneurysms involving both coronary sinuses of Valsalva. J Am Soc Echocardiogr. 2010 Apr;23(4):458.e7-9.
[38] Zhang JP, Meng H, Wang H. Dissecting Aneurysm of the Interatrial and Interventricular Septum with Concomitant Ventricular Septal Defect-Multimodality Cardiac Imaging and Surgical Repair. Echocardiography. 2016 Jun;33(6):932-935.
[39] Salazar J, Gutierrez A, Cay E, et al. Cerebral embolism and thrombus in a membranous interventricular septal aneurysm. Ann Thorac Surg. 2003 Jul;76(1):286-7.
[40] Bakr L, Al-Jadaan M, Younes M. An interventricular membranous septal aneurysm obstructing the right ventricle outflow tract in a five-year-old boy: a case report. J Cardiothorac Surg. 2020;15:297.
Discussion Board
Winners

Javier Cortejoso Spain Physician

Aysegul Ozel Turkey Physician

doğa öcal Turkey Physician

Ionut Valcea Romania Physician
Anna Zhampeissova Kazakhstan Physician