Case of the Week #570
*Department Obstetrics Gynecology, Rambam Medical Center, Haifa, Israel; **St Mary's Medical Center, San Francisco, California, USA
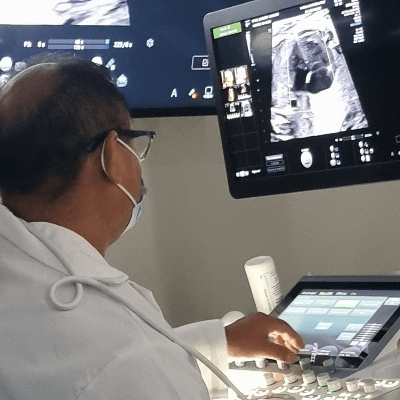
This ultrasound was obtained at 19 weeks of gestation.
View the Answer Hide the Answer
Answer
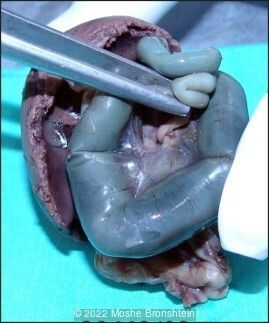
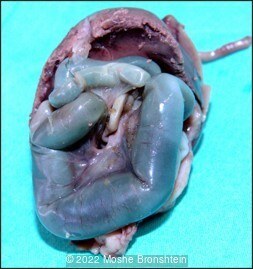
Prenatal imaging was concerning for a small bowel obstruction. Autopsy revealed an internal hernia through the mesentery of the small bowel.

Discussion
Fetal bowel dilatation is characterized by fluid-filled intestinal loops which measure at least 7mm in diameter at any time during pregnancy [1]. Dilated bowel on ultrasound is suggestive of intestinal malformation or obstruction. It is most commonly caused by intestinal atresia and meconium peritonitis, but can also be a result of malrotation with volvulus, anorectal malformation, or Hirschsprung’s disease [1-3]. In a review of 40 cases with prenatal bowel dilation, half were found to have intestinal malformations and these patients were more likely to have associated polyhydramnios, fetal ascites, enlarged stomach, and echogenic bowel on prenatal ultrasound [1].
This case is unique in that the dilated bowel identified prenatally was found at autopsy to be caused by an internal hernia through the mesentery of the small bowel. Congenital internal hernias are rare. In a study reviewing 1827 patients who underwent surgery for small and large bowel obstructions, 10 (0.5%) were found to be due to congenital internal hernia [4]. Internal hernias are classified based on location: paraduodenal, pericecal, foramen of Winslow, transmesenteric, transmesocolic, intersigmoid and retroanastomotic [5]. Among internal hernias, the incidence of congenital transmesenteric hernias ranges from 60% in some studies [4], to 5-10% in others [6,7]. The etiology of mesenteric defects is poorly understood. Hypotheses include regression of the dorsal mesentery, developmental enlargement of a hypovascular area, rapid lengthening of a segment of mesentery and compression of the mesentery by the colon during fetal midgut herniation [5,8,9].
We reviewed the literature for all cases of congenital transmesenteric internal hernias in the past 15 years. In neonates <30 days of age, 17 cases have been reported (Table 1) [5,8-20]. These infants often present with bilious vomiting and abdominal distension. The defect is most commonly located in the terminal ileal mesentery and measures 1.5 – 4cm in size. Nearly 60% had small bowel necrosis or ischemia and approximately 12% had perforation. Four neonates had associated conditions including cystic fibrosis, cardiac anomalies, and microcolon, and approximately 40% of neonates were born preterm. Survival rate was 82%, and of the infants who died, two were born preterm and one had a multiple anomalies.
Prenatal diagnosis of small bowel obstruction due to internal hernia has not been reported. Imaging signs of internal hernia are non-specific and thus pre-operative diagnosis is rare [15]. In the fetal period, ascites [5] or non-reassuring fetal status [15] may be identified, prompting delivery and additional post-natal evaluations.
|
Study
|
GA birth
|
Prenatal course
|
Age at presentation
|
SeX
|
symptoms
|
Surgical findings
|
Necrosis / perforation
|
surgical procedure
|
associated conditions
|
survived (yes/no)
|
|---|---|---|---|---|---|---|---|---|---|---|
|
GA: gestational age; wk: week; NA: not available; M: male; F: female; VSD: ventricular septal defect
|
||||||||||
|
Adnen 2015
|
term
|
NA
|
9 days
|
M
|
abdominal distension, delayed passage of meconium
|
4cm defect at terminal ileum
|
none
|
closure of mesenteric defect
|
none
|
Y
|
|
Batsis 2015
|
term
|
NA
|
5 days
|
M
|
bilious emesis, abdominal distension
|
defect at ligament of Treitz
|
none
|
closure of mesenteric defect
|
none
|
Y
|
|
Elmadi 2014
|
NA
|
NA
|
4 days
|
NA
|
bilious emesis, abdominal distension
|
+ necrosis
|
bowel resection, primary anastomosis
|
none
|
Y
|
|
|
Felizes 2017
|
34wk
|
Ascites
|
1 day
|
F
|
abdominal distension, respiratory compromise
|
defect 20cm from ileocecal valve
|
none
|
bowel resection, ostomy
|
Cystic fibrosis
|
Y
|
|
Hirata 2015
|
22wk
|
NA
|
9 days
|
M
|
bilious emesis, abdominal distension
|
1.5cm defect at terminal ileum
|
+perforation
|
Autopsy
|
none
|
N
|
|
Hirata 2015
|
28wk
|
NA
|
31 days
|
M
|
feeding intolerance, abdominal distension
|
3cm defect at terminal ileum
|
+ischemia
|
bowel resection, ostomy
|
Aortic coarctation, VSD
|
N
|
|
Kylat 2017
|
24wk
|
fetal bradycardia, suspected cord prolapse
|
17 days
|
F
|
feeding residuals, abdominal distension
|
+necrosis
|
bowel resection, ostomy
|
none
|
Y
|
|
|
Lange 2015
|
26wk
|
NA
|
3 days
|
NA
|
abdominal distension
|
defect at terminal ileum
|
+necrosis
|
bowel resection, ostomy
|
none
|
Y
|
|
Lange 2015
|
term
|
NA
|
9 hours
|
NA
|
abdominal distension, abdominal wall erythema
|
defect in distal small bowel
|
+necrosis
|
bowel resection, ostomy
|
none
|
Y
|
|
Leopold 2016
|
32wk
|
decreased fetal movements
|
1 day
|
F
|
abdominal mass
|
defect at terminal ileum
|
+necrosis
|
bowel resection, ostomy
|
none
|
Y
|
|
Malit 2012
|
29wk
|
twins, knotted umbilical cord
|
4 days
|
NA
|
bilious emesis, abdominal distension
|
4cm defect at terminal ileum
|
none
|
bowel resection, ostomy
|
microcolon
|
Y
|
|
Mandhan 2015
|
NA
|
NA
|
5 days
|
F
|
bilious emesis, abdominal distension, no stool
|
2cm defect at distal ileum
|
none
|
closure of mesenteric defect
|
none
|
Y
|
|
Mandhan 2015
|
NA
|
NA
|
5 hours
|
M
|
tachypnea, abdominal distension
|
defect at terminal ileum
|
+perforation
|
bowel resection, primary anastomosis
|
none
|
Y
|
|
Nouira 2011
|
term
|
NA
|
1 day
|
M
|
bilious emesis, abdominal distension
|
defect at distal ileum
|
+necrosis
|
bowel resection, primary anastomosis
|
none
|
Y
|
|
Page 2008
|
term
|
NA
|
1 day
|
M
|
bilious emesis, abdominal distension
|
defect at distal ileum
|
none
|
closure of mesenteric defect
|
none
|
Y
|
|
Sharma 2019
|
term
|
NA
|
7 days
|
M
|
bilious emesis, abdominal distension
|
4cm defect at sigmoid mesocolon
|
none
|
closure of mesenteric defecy
|
none
|
Y
|
|
Tamba 2021
|
term
|
umbilical cord hernia, VSD, aortic transposition
|
3 days
|
M
|
hematochezia
|
defect at terminal ileum
|
+necrosis
|
bowel resection, ostomy
|
umbilical cord hernia, VSD, aortic transposition
|
N
|
References
[1] Xu S, Zhong W, Shen Z, et al. Analysis of the clinical outcomes of fetal bowel dilatation combined with other abnormal ultrasonographic features. J Matern Fetal Neonatal Med. 2019 Mar;32(6):992-996.
[2] Richards C, Holmes SJ. Intestinal dilatation in the fetus. Arch Dis Child Fetal Neonatal Ed. 1995 Mar; 72(2): F135–F138.
[3] Rubio EI, Blask AR, Badillo AT, et al. Prenatal magnetic resonance and ultrasonographic findings in small-bowel obstruction: imaging clues and postnatal outcomes. Pediatr Radiol. 2017 Apr;47(4):411-421.
[4] Fan HP, Yang AD, Chang YJ, et al. Clinical spectrum of internal hernia: a surgical emergency. Surg Today. 2008;38(10):899-904.
[5] Felizes A, Morgado M, Janeiro M, et al. Congenital transmesenteric hernia presenting as neonatal ascites. J Pediatr Surg Case Rep. 2018;28:30-32.
[6] Hansmann, GH, Morton, SA. Intra-Abdominal Hernia: Report of a case and review of the literature. Arch Surg. 1939;39(6):973-986.
[7] Ghiassi S, Nguyen SQ, Divino CM, et al. Internal hernias: clinical findings, management, and outcomes in 49 nonbariatric cases. J Gastrointest Surg. 2007 Mar;11(3):291-5
[8] Malit M, Burjonrappa S. Congenital mesenteric defect: Description of a rare cause of distal intestinal obstruction in a neonate. Int J Surg Case Rep. 2012; 3(3): 121–123.
[9] Lange P, Parrish D. Congenital internal hernias: rare cause of intestinal obstruction in newborns. J Clin Neonatol. 2015 Apr;4(2):138-141.
[10] Adnen H, Aida B, Serra B, et al. mesenteric defect with internal herniation: a rare cause of bowel obstruction in newborn. Fetal Pediatr Pathol. 2015;34(4):207-11.
[11] Batsis ID, Okito O, Meltzer JA, et al. Internal hernia as a cause for intestinal obstruction in a newborn. J Emerg Med. 2015 Sep;49(3):277-80.
[12] Elmadi A, Lechqar M, El Biache I, et al. Trans-mesenteric hernia in infants: report of two cases. J Neonatal Surg. 2014 Jul-Sep; 3(3): 29.
[13] Hirata K, Kawahara H, Shiono N, et al. Mesenteric hernia causing bowel obstruction in very low-birthweight infants. Pediatr Int. 2015;57(1):161-3.
[14] Kylat RI. Internal hernia masquerading as necrotizing enterocolitis. Front Pediatr. 2017; 5: 225.
[15] Leopold S, Al-Qaraghouli M, Hussain N, et al. Magnetic resonance imaging diagnosis of volvulus through mesenteric defect in neonate. AJP Rep. 2016 Apr; 6(2): e239–e242.
[16] Mandhan P, Alshahwani N, Al-Balushi Z, et al. Congenital mesenteric hernia in neonates: Still a dilemma. Afr J Paediatr Surg. 2015 Jul-Sep; 12(3): 203–207.
[17] Nouira F, Dhaou BM, Charieg A, et al. Small bowel obstruction caused by congenital transmesenteric defect. Afr J Paediatr Surg. 2011 Jan-Apr;8(1):75-8.
[18] Page MP, Robert L Ricca, Andrew S Resnick, et al. Newborn and toddler intestinal obstruction owing to congenital mesenteric defects. J Pediatr Surg. 2008 Apr;43(4):755-8.
[19] Sharma K, Dhua A, Thomas D, et al. Congenital sigmoid mesocolic defect as a cause of neonatal intestinal obstruction. BMJ Case Rep. 2019 Aug 28;12(8):e230253.
[20] Tamba RP, Wiradeni A. Management of internal hernia in neonates with multiple heart diseases: a case report. The New Ropanasuri Journal of Surgery. 2021; Jun;6(1):24-26.
Discussion Board
Winners

Javier Cortejoso Spain Physician

Ana Ferrero Spain Physician

Oskar Sylwestrzak Poland Physician

Vladimir Lemaire United States Physician

Michal Michna Slovakia Physician
Halil Mesut Turkey Physician

Anita Silber Israel Physician

Ta Son Vo Viet Nam Physician

Phùng Hiếu Viet Nam Physician

LILY LI China Physician
JOSE DERBY MEJIA FERNANDEZ Peru Physician

kim lowman United States Sonographer