Case of the Week #567
(1) Femicare, Center of prenatal ultrasonographic diagnostics, Martin, Slovakia; (2) Centro Médico Recoletas. Valladolid. Spain
Case Report: A 33-year-old primigravida, with non-contributive history, was sent to our office at 20 weeks of gestation. Our ultrasound examination revealed following findings:



View the Answer Hide the Answer
Answer
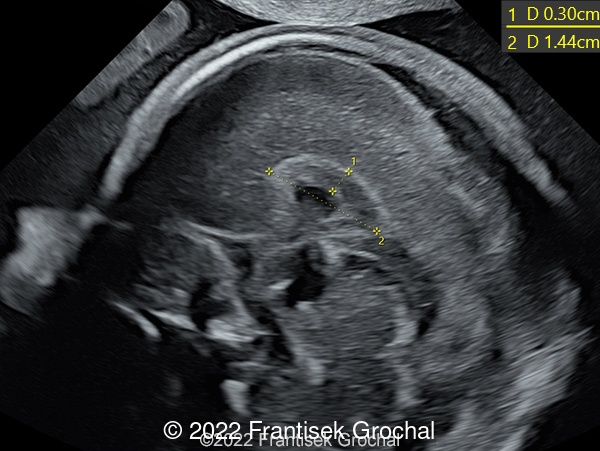
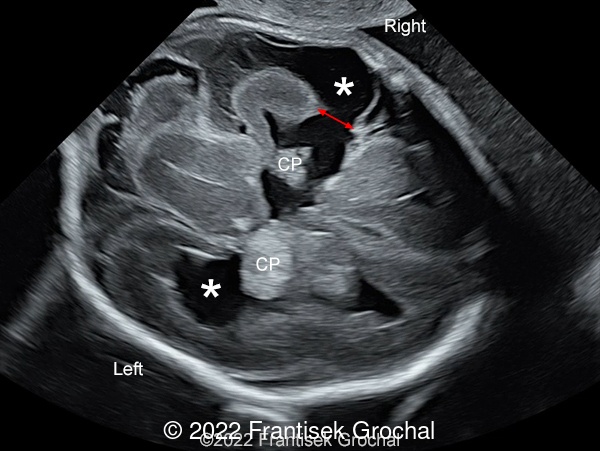
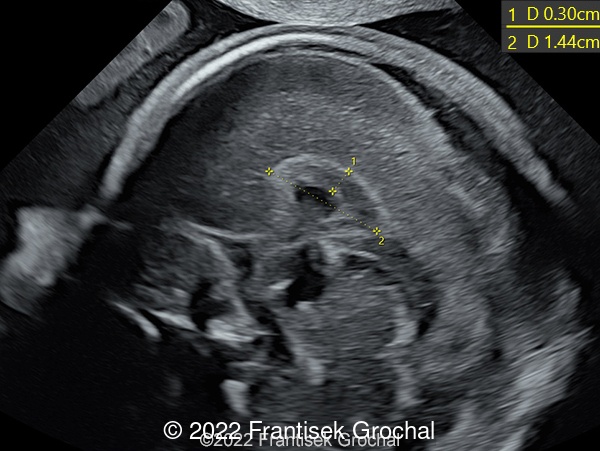
We present a case of Schizencephaly. Our ultrasound revealed the following:
- Right sided schizencephaly characterized as an open-lip type (type II) with a large cortical defect measuring 6.7 mm
- Bilateral enlargement of lateral cerebral ventricles (12-13 mm)
- Thickened and short corpus callosum
Due to the poor neurological prognosis the parents opted for termination of the pregnancy.



Discussion
The term "malformation of cortical development" was first introduced in 1996 to describe a group of disorders that usually present with neurodevelopmental delay and epilepsy, caused by alterations in the orderly process of generation and maturation of the cerebral cortex [1]. Until recently this term was used to refer to neuronal migration disorders. The current classification of cortical developmental malformations includes defects caused by alterations in one of the three steps of the process: neuronal/glial proliferation, neuronal migration, and cortical organization [2]. Malformations secondary to abnormal postmigrational development are polymicrogyria and schizencephaly (group III.A), cortical dysgenesis secondary to inborn errors of metabolism (group III.B), focal cortical dysplasias (group III.C), and postmigrational microcephaly (group III.D) [3]. In this group of malformations, previously known as disorders of cortical organization, neurons that have reached the cortex fail to organize normal connections [3].
These overlapping maturational phases occur relatively late in pregnancy and do not end until after delivery, making a definitive diagnosis difficult during pregnancy. Ultrasound signs suggestive of cortical development anomalies are early abnormal sulcation, irregular ventricular walls, parenchymal nodules, thin and irregular or underdeveloped cortex, an enlarged hemisphere, and cortical clefting [4,5]. Ultrasound is the method of choice for examination of fetal brain anatomy including the malformations of cortical development [5]. However, some aspects of brain maturation and myelination are better assessed with Magnetic Resonance Imaging (MRI) [6], especially with maternal obesity, challenging fetal position, decreased amniotic fluid or technical difficulties such as near-field reverberation artifact [7].
The term schizencephaly, sometimes called agenetic porencephaly, describes an abnormality of the brain in which cortical gray matter-lined clefts extend through the entire cerebral mantle, from the ependymal lining of the lateral ventricles to the pial covering of the cortex [8]. First described by Wilmarth in 1887 [9], the term was coined from the Greek word "schizen", 'to divide', and introduced by Yakovlev and Wadsworth in 1946, based on their work on cadavers [10]. They described two types of schizencephaly: type I (closed-lip), a fused cleft that prevented the passage of cerebrospinal fluid, and type II (open-lip), a cleft of irregular width permitting cerebrospinal fluid to pass between the ventricular cavity and subarachnoid space [10, 11].
Schizencephaly is a rare birth defect. A study in a Californian population of more than 4 million births found a prevalence of 1.54 in 100,000 births [12], which is similar to a study by Howe et al in the United Kingdom (1.48 in 100 000 births) [13].
The causes of schizencephaly are heterogeneous, and have been associated with young parental age, lack of prenatal care, teratogens (warfarin, alcohol, and cocaine), infections (cytomegalovirus and herpes virus), maternal trauma, monozygotic twin interactions, and thrombophilia [12-14]. The association with syndromic pathologies such as chromosomal aneuploidy, single gene defects, and a few syndromes, is probably incidental. In some familial cases, schizencephaly has been linked to mutations in different genes (EMX2, COL4A1, SHH, and SIX3), however, this is uncommon [15-17]. The epidemiologic evidence associating this defect with young maternal age as well as the link with malformations that have a vascular pathogenesis supports the hypothesis that schizencephaly may be both a primary malformation of cortical development, and a disruptive vascular birth defect [8].
Schizencephaly remains a rare antenatal diagnosis, it is only identified antenatally by ultrasound and/or magnetic resonance imaging in 47% of cases, with most cases after 28 weeks gestation [13]. Although the damaging process that causes schizencephaly may occur early in pregnancy, it may not be apparent until later, and is not often detected on the early second-trimester scan. Fetal sonographic findings of this entity were first described in 1986 by Klingensmith in a 15-year-old primigravida during her 31st menstrual week [18]. Ventriculomegaly is often the first sign detected [19], being easier to diagnose open lip cases than fused ones. They are displayed as wide clefts of cerebrospinal fluid communicating the lateral ventricles and subarachnoid spaces often lined by echogenic tissue [18, 20-29]. Closed-lipped clefts may be suggested in the presence of parallel echogenic tissue extending from the lateral ventricle to the extraaxial fluid space [26, 30]. The cerebral clefts can be bilateral or unilateral, symmetrical or asymmetrical, small or large, and are commonly located in the perisylvian region. Findings visualized by MRI are identical to those described by ultrasound, with better definition of the clefts and better visualization of associated abnormalities such as polymicrogyria and heterotopic gray matter [19, 20, 24-27, 29].
Although schizencephaly can occur in isolation, other brain anomalies are commonly associated [12]. The most frequent are absence of the septum pellucidum, agenesis or dysgenesis of the corpus callosum, ventriculomegaly, gyral malformations (including polymicrogyria and gray matter heterotopias), arachnoid cyst, posterior fossa abnormalities, and optic nerve hypoplasia (septo-optic dysplasia) [12]. Septo-optic dysplasia has been associated with a wide variety of central nervous system (CNS) malformations, and it is possible that those patients who also have schizencephaly represent a distinct subgroup of patients with this disease, termed septo-optic dysplasia plus [31]. One-third of affected patients have a non-CNS abnormality, most thought to be due to vascular disruption, such as gastroschisis, bowel atresia, and amniotic band syndrome [12].
The differential diagnosis between intracranial defects containing cerebrospinal fluid include both developmental and destructive lesions. They include arachnoid cyst, ventriculomegaly, monoventricle of alobar holoprosencephaly, porencephalic cysts, and hydranencephaly [23]. Identification of the gray‑matter lining of the cleft is critical in differentiating schizencephaly from porencephaly and arachnoid cysts, while hydranencephaly and holoprosencephaly can be excluded by detection of normal basal ganglia structures and midline falx [30].
Clinical manifestations of schizencephaly most often include varying degrees of developmental delay, motor impairment, and seizures [23, 32]. The severity of motor and mental disorders is directly related to the extent and location of the anatomical defect [33], but the presence or severity of epilepsy is not [34]. Open-lip bilateral clefts usually result in the most significant impairment, while unilateral closed clefts have a less severe clinical presentation. Sometimes, an apparently open cleft prenatally may become closed postnatally [26].
References
[1] Barkovich AJ, Kuzniecky RI, Dobyns WB, et al. A classification scheme for malformations of cortical development. Neuropediatrics. 1996 Apr;27(2):59-63. PMID: 8737819.
[2] Tortori-Donati P, Rossi A, and Biancheri R. Brain Malformations. In: Paolo Tortori-Donati and Andrea Rossi, ed. Pediatric Neuroradiology. Springer-Verlag, Berlin Heidelberg, 2005; pages 71-198.
[3] Barkovich AJ, Guerrini R, Kuzniecky RI, et al. A developmental and genetic classification for malformations of cortical development: update 2012. Brain. 2012 May;135(Pt 5):1348-69. PMID: 22427329; PMCID.
[4] Malinger G, Toi A, Ben-Sira L a et al. Malformations of cortical development. In: Timor-Tritsch IE, Monteagudo A, Pilu G and Malinger G, ed. Ultrasonography of the Prenatal Brain, 3rd ed. The McGraw-Hill Companies, Inc, 2012; pages 247-282.
[5] Malinger G, Kidron D, Schreiber L, et al. Prenatal diagnosis of malformations of cortical development by dedicated neurosonography. Ultrasound Obstet Gynecol. 2007 Feb;29(2):178-91. PMID: 17219377.
[6] Paus T, Collins DL, Evans AC, L et al. Maturation of white matter in the human brain: a review of magnetic resonance studies. Brain Res Bull. 2001 Feb;54(3):255-66. PMID: 11287130.
[7] Salomon LJ, Garel C. Magnetic resonance imaging examination of the fetal brain. Ultrasound Obstet Gynecol. 2007 Dec;30(7):1019-32. PMID: 17994613.
[8] Barkovich AJ and Raybaud C. Congenital Malformations of the Brain and Skull. In: Barkovich AJ and Raybaud, C, ed. Pediatric neuroimaging, 6th edition. Wolters Kluwer, Philadelphia, 2018.
[9] Wilmarth WA. Presentation to the Philadelphia Neurological Society. J Nerv Ment Dis 1887;14:395-407.
[10] Yakovlev PI, Wadsworth RC. Schizencephalies; a study of the congenital clefts in the cerebral mantle; clefts with fused lips. J Neuropathol Exp Neurol. 1946 Apr;5:116-30. PMID: 21026933.
[11] Yakovlev PI, Wadsworth RC. Schizencephalies; a study of the congenital clefts in the cerebral mantle; clefts with hydrocephalus and lips separated. J Neuropathol Exp Neurol. 1946 Jul;5(3):169-206. PMID: 20993391.
[12] Curry CJ, Lammer EJ, Nelson V, et al. Schizencephaly: heterogeneous etiologies in a population of 4 million California births. Am J Med Genet A. 2005 Aug 30;137(2):181-9. PMID: 16059942.
[13] Howe DT, Rankin J, Draper ES. Schizencephaly prevalence, prenatal diagnosis and clues to etiology: a register-based study. Ultrasound Obstet Gynecol. 2012 Jan;39(1):75-82. PMID: 21647999.
[14] Dies KA, Bodell A, Hisama FM, et al. Schizencephaly: association with young maternal age, alcohol use, and lack of prenatal care. J Child Neurol. 2013 Feb;28(2):198-203. PMID: 23266945
[15] Tietjen I, Bodell A, Apse K, et al. Comprehensive EMX2 genotyping of a large schizencephaly case series. Am J Med Genet A. 2007 Jun 15;143A(12):1313-6. PMID: 17506092.
[16] Sato Y, Shibasaki J, Aida N, H et al. Novel COL4A1 mutation in a fetus with early prenatal onset of schizencephaly. Hum Genome Var. 2018 Apr 24;5:4. PMID: 29760938
[17] Hehr U, Pineda-Alvarez DE, Uyanik G, et al. Heterozygous mutations in SIX3 and SHH are associated with schizencephaly and further expand the clinical spectrum of holoprosencephaly. Hum Genet. 2010 Mar;127(5):555-61. PMID: 20157829
[18] Klingensmith WC 3rd, Cioffi-Ragan DT. Schizencephaly: diagnosis and progression in utero. Radiology. 1986 Jun;159(3):617-8. PMID: 3517949.
[19] Denis D, Maugey-Laulom B, Carles D, et al. Prenatal diagnosis of schizencephaly by fetal magnetic resonance imaging. Fetal Diagn Ther. 2001 Nov-Dec;16(6):354-9. PMID: 11694738.
[20] Lituania M, Passamonti U, Cordone MS, et al. Schizencephaly: prenatal diagnosis by computed sonography and magnetic resonance imaging. Prenat Diagn. 1989 Sep;9(9):649-55. PMID: 2678087.
[21] Komarniski CA, Cyr DR, Mack LA, et al. Prenatal diagnosis of schizencephaly. J Ultrasound Med. 1990 May;9(5):305-7. PMID: 2188013.
[22] Ceccherini AF, Twining P, Variend S. Schizencephaly: antenatal detection using ultrasound. Clin Radiol. 1999 Sep;54(9):620-2. PMID: 10505999.
[23] Oh KY, Kennedy AM, Frias AE Jr, et al. Fetal schizencephaly: pre- and postnatal imaging with a review of the clinical manifestations. Radiographics. 2005 May-Jun;25(3):647-57. PMID: 15888615.
[24] Edris F, Kielar A, Fung KF, et al. Ultrasound and MRI in the antenatal diagnosis of schizencephaly. J Obstet Gynaecol Can. 2005 Sep;27(9):864-8. PMID: 19830952.
[25] Gedikbasi A, Yildirim G, Saygi S, et al. Prenatal diagnosis of schizencephaly with 2D-3D sonography and MRI. J Clin Ultrasound. 2009 Oct;37(8):467-70. PMID: 19536862.
[26] Lee W, Comstock CH, Kazmierczak C, et al. Prenatal diagnostic challenges and pitfalls for schizencephaly. J Ultrasound Med. 2009 Oct;28(10):1379-84. PMID: 19778886
[27] Kutuk MS, Gorkem SB, Bayram A, et al. Prenatal Diagnosis and Postnatal Outcome of Schizencephaly. J Child Neurol. 2015 Sep;30(10):1388-94. PMID: 25535059.
[28] Matsumoto T, Miyakoshi K, Fukutake M, et al. Intracranial sonographic features demonstrating in utero development of hemorrhagic brain damage leading to schizencephaly-associated COL4A1 mutation. J Med Ultrason (2001). 2015 Jul;42(3):445-6. PMID: 26576802.
[29] Harada T, Uegaki T, Arata K, T et al. Schizencephaly and Porencephaly Due to Fetal Intracranial Hemorrhage: A Report of Two Cases. Yonago Acta Med. 2018 Feb 5;60(4):241-245. PMID: 29434494.
[30] Kline-Fath BM. Supratentorial Anomalies. In: Kline-Fath BM, Bulas DI and Bahado-Singh R, ed. Fundamental and Advanced Fetal Imaging. Ultrasound and MRI. Wolters Kluwer Health, Philadelphia, 2015; pages 345-423.
[31] Miller SP, Shevell MI, Patenaude Y, et al. Septo-optic dysplasia plus: a spectrum of malformations of cortical development. Neurology. 2000 Apr 25;54(8):1701-3. PMID: 10762523.
[32] Hung PC, Wang HS, Chou ML, et al. Schizencephaly in children: A single medical center retrospective study. Pediatr Neonatol. 2018 Dec;59(6):573-580. PMID: 29371079.
[33] Barkovich AJ, Kjos BO. Schizencephaly: correlation of clinical findings with MR characteristics. AJNR Am J Neuroradiol. 1992 Jan-Feb;13(1):85-94. PMID: 1595498
{34] Granata T, Battaglia G, D'Incerti L, F et al. Schizencephaly: neuroradiologic and epileptologic findings. Epilepsia. 1996 Dec;37(12):1185-93. PMID: 8956850.
Discussion Board
Winners

Paula Melone United States Physician

Dianna Heidinger United States Sonographer

Seadet Zeynalova Azerbaijan Physician

Marina Bagdasaryan Russian Federation Physician

Fatih ULUC Turkey Physician

Umber Agarwal United Kingdom Maternal Fetal Medicine

Igor Yarchuk United States Sonographer

Iuliia Iudina Russian Federation Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Mayank Chowdhury India Physician

filiz halici öztürk Turkey Physician

Oskar Sylwestrzak Poland Physician

Vladimir Lemaire United States Physician
Shilpen Gondalia India Physician
Ivan Ivanov Russian Federation Physician

Boujemaa Oueslati Tunisia Physician

Sara Abdallah Salem Egypt Physician
Halil Mesut Turkey Physician

Rushina Patel United States Sonographer
Anita Silber Israel Physician

lan nguyen xuan Viet Nam Physician

Olivia Ionescu United Kingdom Physician
Rebecca Evans Australia Sonographer

Suat İnce Turkey Physician

Elena Andreeva Russian Federation Physician

santosh shahare United States Physician

ALBANA CEREKJA Italy Physician

Selvanandhini Gopalasundaram India Physician

Murat Cagan Turkey Physician
Rasha Abo Almagd Egypt Physician

Ionut Valcea Romania Physician
José Lambertino Colombia Physician

Ahmed Abujaber Canada Physician
KHALED RAMADAN Egypt Physician
TEJAS TAMHANE India Physician

Abdullah Alnoman Canada Physician

mahmoud elbohy Egypt Physician

Seda Cam Turkey Physician

Miguel Sanchez Mexico Physician
Anna Zhampeissova Kazakhstan Physician

Michael Hussey United States Physician

andrea tavares de oliveira Brazil Physician
Tuấn Sơn Nông Viet Nam Physician

Sushant Jain United States Medical Student

Halil Korkut Dağlar Turkey Physician

Katarína Pitoňáková Czech Republic Physician

Deborah Buchanan United States Sonographer
Manojkumar K India Physician

Atefe Sh Indonesia Sonographer

Xavier Pombar United States Physician

Sumit Singhania India Radiologist

Aditi Goundan India Physician