Case of the Week #563
Tula Regional Perinatal Center
Posting Dates: July 15 - July 30, 2022
Reviewer: Irina Tihonenko
Case Report: A 33-year-old woman with no past medical history was followed at the Antenatal Clinic starting at 8 weeks gestation. She previously delivered two healthy children. Combined first-trimester screening was negative. The 2nd trimester screening done at 20-21 weeks showed fetal growth was consistent with gestational age. The patient had mild infection with COVID-19 at 24 weeks' gestation, thus underwent ultrasound examinations once every 3-4 weeks according to current guidelines. The following images were obtained at 33-34 weeks.



View the Answer Hide the Answer
Answer
We present a case of antenatal left testicular torsion with irreversible sclerotic changes.
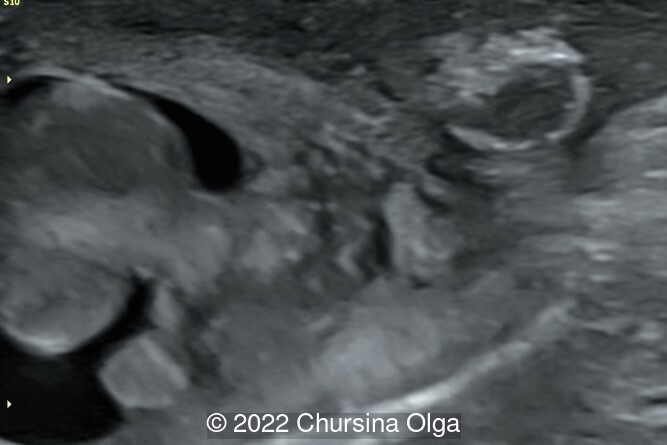
Our ultrasound examination revealed appropriate fetal growth, as well as normal amniotic fluid and placenta. Examination of the fetal scrotum showed a discrepancy in size between the right and left with the left side being smaller (Image 1). A rounded bean-shaped mass measuring 8.8 x 4.6 mm with a thick, hyperechogenic fibrous contour was detected in the left half of the scrotum. The normal structure of the left testis is not detected. The right fetal testis was normal (Image 2). On doppler imaging, there is absence of flow in the left hemiscrotum, and normal flow on the right side (Image 3). The left testicular appendages are not visualized. On dynamic observation, there is no peristaltic movement in the left half of the scrotum. The right scrotum shows a normal testicular structure with appendages. There is no hydrocele in the scrotum (Image 3).
- Image 1: Asymmetry of the left and right halves of the fetal scrotum
- Image 2: Bean-shaped formation of the left half of the fetal scrotum, the right testicle is normal
- Image 3: Absence of blood flow in the left half of the fetal scrotum
- Video 1: Hyperechoic contour of the formation of the left half of the fetal scrotum, the right testicle is normal
- Video 2: Lack of blood flow in the left half of the fetal scrotum. No peristalsis identified.
The diagnosis of left testicular torsion with atrophy was made. Repeat ultrasound at 37-38 weeks' gestation showed the same findings in the scrotum
Postnatal ultrasound examination of the scrotum confirmed the prenatal diagnosis. The left half of the scrotum had no normal testicular structure. The testis was structureless with a hyperechogenic sclerotic contour, avascular, and there was no differentiation of the parenchyma and testicular appendage. The right testis was normal in size and structure (Image 1,2).

Given the presumed chronicity of the torsion, surgical treatment was not indicated. The prognosis for left testicular function is unfavorable, but, given the normal parameters of the right testicle, the reproductive potential should be intact.
Discussion
Perinatal testicular torsion is defined as occurring before 30 days of life. This includes both prenatal cases of testicular torsion as well as those diagnosed after birth. The prevalence of perinatal testicular torsion has been estimated at 1 in 80,000 male deliveries [1]. Approximately 80-85% of perinatal testicular torsion is identified at birth, suggesting the process began prenatally [2,3]. While most cases are unilateral, approximately 7-18% of cases are bilateral [2,3].
There are rare case reports of prenatal diagnosis of testicular torsion [1,4,5]. Testicular torsion is more commonly detected in the third trimester [1,4,5], though there have been reports of earlier events [6]. The presence of hydrocele can be an early sign of testicular torsion [7]. Prenatal ultrasound can show a “double ring hemorrhage,” which is an enlarged testes surrounded by two hypoechogenic fluid concentric layers [5]. This double layer is explained by accumulation of hemorrhagic fluid between the visceral and parietal layers of the tunicae vaginalis and outside the tunica vaginalis [5].
The differential diagnosis of testicular torsion includes inguinal hernia, scrotal tumor, orchiepididymitis, and torsion of the testicular-epididymal appendage [4].
The management of perinatal testicular torsion is debated. In a review of the literature including 59 cases of perinatal testicular torsion, there was a 0% salvage rate of the affected testicle [1]. Other series report a 6-7% salvage rate [2,3], though these cases were postnatal in onset [2] or salvage of a contralateral torsed gonad that was not suspected pre-operatively [3]. The most compelling reason for urgent exploration in neonates with unilateral torsion is suspected torsion of the contralateral viable gonad without obvious clinical or radiographic findings [2,3,8,9]. A prenatal diagnosis of unilateral torsion is not an indication for delivery unless there is imaging evidence that the torsion occurred within 24 hours. In cases of bilateral torsion diagnosed after 34 weeks, induced delivery and neonatal surgical intervention is advocated to attempt preservation of at least one testis [1].
References
[1] Melcer Y, Mendlovic S, Klin B et al. Fetal diagnosis of testicular torsion: what shall we tell the parents? Prenat Diagn. 2015 Feb;35(2):167-73.
[2] Kaye JD, Levitt SB, Friedman SC, et al. Neonatal torsion: a 14-year experience and proposed algorithm for management. J Urol. 2008 Jun;179(6):2377-83.
[3] Abraham MB, Charles A, Gera P, et al. Surgically managed perinatal testicular torsion: a single centre experience. J Matern Fetal Neonatal Med. 2016;29(8):1265-8.
[4] Devesa R, Muñoz A, Torrents M, et al. Prenatal diagnosis of testicular torsion. Ultrasound Obstet Gynecol. 1998 Apr;11(4):286-8.
[5] Herman A, Schvimer M, Tovbin J, et al. Antenatal sonographic diagnosis of testicular torsion. Ultrasound Obstet Gynecol. 2002 Nov;20(5):522-4.
[6] Sauvestre F, André G, Harran MH, et al. Prenatal Testicular Torsion: Not Always in the Late Third Trimester. Urology. 2016 Mar;89:132-3.
[7] Arena F, Nicòtina PA, Romeo C, et al. Prenatal testicular torsion: ultrasonographic features, management and histopathological findings. Int J Urol. 2006 Feb;13(2):135-41.
[8] Roth CC, Mingin GC, Ortenberg J. Salvage of bilateral asynchronous perinatal testicular torsion. J Urol. 2011 Jun;185(6 Suppl):2464-8.
[9] Yerkes EB, Robertson FM, Gitlin J, et al. Management of perinatal torsion: today, tomorrow or never? J Urol. 2005 Oct;174(4 Pt 2):1579-82.
With thanks to the great Philippe Jeanty in whose article I found the correct diagnosis
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Danilo Feitosa Brazil Physician

Fatih ULUC Turkey Physician

Umber Agarwal United Kingdom Maternal Fetal Medicine

Igor Yarchuk United States Sonographer

Cem Sanhal Turkey Physician

Ana Ferrero Spain Physician

Mayank Chowdhury India Physician

filiz halici öztürk Turkey Physician

Oskar Sylwestrzak Poland Physician

DAVID BEAUMONT United Kingdom Physician

Lames Ghith United States Physician

Tatiana Koipish Belarus Physician

Sara Abdallah Salem Egypt Physician
Halil Mesut Turkey Physician

Rushina Patel United States Sonographer
Rebecca Evans Australia Sonographer

Suat İnce Turkey Physician

Rime NSEIR France Physician
Liem Dang Le Viet Nam Physician

Elena Andreeva Russian Federation Physician

Muradiye YILDIRIM Turkey Physician

Ta Son Vo Viet Nam Physician

ALBANA CEREKJA Italy Physician
SAMUEL GELVEZ TELLEZ Colombia Physician

Murat Cagan Turkey Physician
Rasha Abo Almagd Egypt Physician

Ionut Valcea Romania Physician
José Lambertino Colombia Physician

Elham Eghbali Iran, Islamic Republic of Radiologist
KHALED RAMADAN Egypt Physician

mahmoud elbohy Egypt Physician

Kathrine Montagne United States Sonographer

Ramesh Giti United States Physician

TATIANA VOLKOVA Kyrgyzstan Physician

SUSAN FORDEN Australia Sonographer