Discussion
Deficiency of the clavicle encompasses a wide spectrum of anomalies, ranging from mild hypoplasia to total agenesis. Its presence should prompt an adequate family history, as well as a search for other abnormalities that may identify a specific syndrome or skeletal dysplasia. The most characteristic disorder with clavicular aplasia/hypoplasia is cleidocranial dysplasia (CCD, OMIM # 119600), which is a skeletal dysplasia characterized by delayed closure of the cranial sutures, hypoplastic or aplastic clavicles, and multiple dental abnormalities. This classical cleidocranial dysplasia is considered the most severe form of the “cleidocranial dysplasia spectrum disorder,” a clinical continuum ranging from isolated dental anomalies without skeletal features to the classic dysplasia [1]. Therefore, signs and symptoms can vary widely in severity, even within the same family.
Cleidocranial dysplasia is also known as cleidocranial dysostosis, osteodental dysplasia, Marie-Sainton disease, and Scheuthauer-Marie-Sainton syndrome. The disorder takes the eponymous of Pierre Marie and Paul Sainton, two French physicians who characterized the disease in 1898, naming it “Dysostose Cléido-Crânienne Héréditaire” [2]. Previously, in 1871, Gustav Scheuthauer, an Austro-Hungarian surgeon, had described the combination of rudimentary clavicles with cranial abnormalities in an adult [3], and it is possible that Johann Friedrich Meckel the Elder described the disease as early as 1760.
The estimated prevalence of cleidocranial dysplasia is 1 per 1,000,000 live births, affecting all ethnic groups [1]. However, this value may be underestimated due to mild cases presenting with relatively inconspicuous clinical symptoms. Some authors report a higher incidence of 1 in 200 000 live births [4].
Cleidocranial dysplasia is inherited in an autosomal dominant manner. Most cleidocranial dysplasia cases (80%) are linked to a mutation in the RUNX2 gene on chromosome 6p21, also known as the CBFA1 [5], which is essential for osteoblast differentiation and, for both membranous and endochondral bone formation during skeletal development [6]. Prenatal diagnosis by molecular genetic testing for pregnancies at increased risk is possible if the pathogenic variant in the family is known. In addition, a CCD-like phenotype has been reported in association with cytogenetic abnormalities of chromosome 8q22 [7].
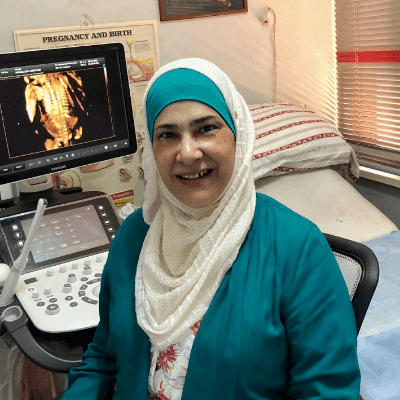
Cleidocranial dysplasia can be diagnosed by ultrasound examination in the offspring of an affected parent [6, 8-10], and as early as 13-14 weeks gestation [9, 10]. In some cases, the diagnosis is made with a negative family history because cleidocranial dysplasia may go unrecognized in the parents until a diagnosis is made on fetal ultrasound [11-13].
The most consistent features are abnormal clavicles, which are short (<5th centile for gestational age), partially, or totally absent [1]. The craniofacial findings include large fontanelles with wide sutures and multiple wormian bones, brachycephalic skull with hypomineralization, frontal bossing, flat occiput, and midfacial hypoplasia with a low nasal bridge and absent nasal bones [4, 12, 14]. Prenatal observation during the first trimester ultrasound exam of nasal hypoplasia/aplasia in chromosomally normal fetuses should prompt a careful search for skeletal dysplasias, and a thorough evaluation of the clavicles [14].
Other features detectable on prenatal ultrasound examination include immaturity of ossification, long bones below the fifth percentile, cervical rib, small thorax with short and obliquely oriented ribs, posterior wedging of thoracic vertebrae, scoliosis, small scapulae, abnormalities of the hands, and underdeveloped vertical hypoplastic iliac wings [9]. In utero, the basic findings leading to the diagnosis are clavicular hypoplasia and short limbs [11].
The differential diagnosis of the cleidocranial dysplasia includes disorders characterized by poor mineralization of the calvarium, such as hypophosphatasia and osteogenesis imperfecta [13], as well as disorders that have congenital clavicular hypoplasia or agenesis as its most characteristic phenotypic finding. Poor or delayed calcification of the calvarium is observed in the perinatal and infantile forms of hypophosphatasia, but neither hypoplasia nor absence of the clavicles has been reported in association with this pathology. Osteogenesis imperfecta should be considered in the differential diagnosis, as poor ossification of the skull can be present in fetuses with this condition; it presents generalized hypomineralization and multiple bone fractures with severe shortening and bowing of the long bones. Other syndromes with congenital clavicular hypoplasia or agenesis include Yunis–Varon syndrome, cleidocranial dysplasia with parietal foramina, pyknodysostosis, mandibulo-acral dysplasia, and osteodysplasty (Melnick-Needles syndrome) [16]. They can be ruled out due to their high bone density. Yunis–Varon syndrome is a severe autosomal recessive disorder characterized by large fontanelles, clavicular hypoplasia, characteristic facial features and/or limb defects. These defects (hypoplasia or absence of thumbs and big toes and distal phalangeal hypoplasia) are not seen in the cleidocranial dysplasia.
Vaginal delivery may increase the risk of intracranial hemorrhage in a fetus with cleidocranial dysplasia, thus some authors advise an elective caesarean section to avoid traumatic head injuries associated with delivery [15]. Despite this, the outcome of the condition is relatively benign and it is not associated with mental retardation or non-harmonic short stature [11].
References
[1] Machol K, Mendoza-Londono R, Lee B. “Cleidocranial Dysplasia Spectrum Disorder.” GeneReviews® 1993-2021. Seattle (WA): University of Washington, Seattle 2006. [Updated 2017 Nov 16]. PMID: 20301686.
[2] Marie P, Sainton P. Sur la dysostose cléido-cranienne héréditaire. Rev Neurol 1898;6:835-838.
[3] Scheuthauer G. Kombination rudimentärer Schlüsselbeine mit Anomalien des Schädels beim erwachsenen Menschen. Allg Wien Med Ztg 1871;16:293-295.
[4] Lachman RS. Taybi and Lachman’s Radiology of Syndromes, Metabolic Disorders, and Skeletal Dysplasias, Fifth Edition. Philadelphia: Mosby Elsevier, 2006. pg 913-915.
[5] Mundlos S, Otto F, Mundlos C, et al. Mutations involving the transcription factor CBFA1 cause cleidocranial dysplasia. Cell. 1997 May 30;89(5):773-9.
[6] Hermann NV, Hove HD, Jørgensen C, et al. Prenatal 3D ultrasound diagnostics in cleidocranial dysplasia. Fetal Diagn Ther. 2009;25(1):36-9. PMID: 19169035.
[7] Brueton LA, Reeve A, Ellis R, et al. Apparent cleidocranial dysplasia associated with abnormalities of 8q22 in three individuals. Am J Med Genet. 1992 Jun 1;43(3):612-8. PMID: 1605259.
[8] Hamner LH 3rd, Fabbri EL, Browne PC. Prenatal diagnosis of cleidocranial dysostosis. Obstet Gynecol. 1994 May;83(5 Pt 2):856-7. PMID: 8159376.
[9] Stewart PA, Wallerstein R, Moran E, et al. Early prenatal ultrasound diagnosis of cleidocranial dysplasia. Ultrasound Obstet Gynecol. 2000 Feb;15(2):154-6. PMID: 10776001.
[10] Hove HD, Hermann NV, Jørgensen C, et al. An echo-poor spine at 13 weeks: an early sign of cleidocranial dysplasia. Fetal Diagn Ther. 2008;24(2):103-5. PMID: 18648208.
[11] Paladini D, Lamberti A, Agangi A, et al. Cleidocranial dysostosis. Prenatal ultrasound diagnosis of a late onset form. Ultrasound Obstet Gynecol. 2000 Jul;16(1):100-1. PMID: 11084978
[12] Hassan J, Sepulveda W, Teixeira J, et al. Prenatal sonographic diagnosis of cleidocranial dysostosis. Prenat Diagn. 1997 Aug;17(8):770-2. PMID: 9267902.
[13] Soto E, Richani K, Gonçalves LF et al. Three-dimensional ultrasound in the prenatal diagnosis of cleidocranial dysplasia associated with B-cell immunodeficiency. Ultrasound Obstet Gynecol. 2006 May;27(5):574-9. PMID: 16619383.
[14] Chen CP, Hung HY, Chang TY, et al. Second-trimester nasal bone hypoplasia/aplasia associated with cleidocranial dysplasia. Prenat Diagn. 2004 May;24(5):399-400. PMID: 15164420.
[15] Nagasaka S, Suzuki K, Saito T, et al. Posterior fossa subdural hematoma in a neonate with cleidocranial dysostosis after a spontaneous vaginal delivery: a case report. Childs Nerv Syst. 2021 Feb;37(2):683-686. PMID: 32504170.
[16] Winer N, Le Caignec C, Quere MP, et al. Prenatal diagnosis of a cleidocranial dysplasia-like phenotype associated with a de novo balanced t(2q;6q)(q36;q16) translocation. Ultrasound Obstet Gynecol. 2003 Dec;22(6):648-51. PMID: 14689542.